HTML
CSS
Anatomy
Physiology
Neurological Disorders
Pain Management
Aviation
Safety
飛機旅行壓力變化對偏頭痛的影響

咽鼓管功能失調的角色
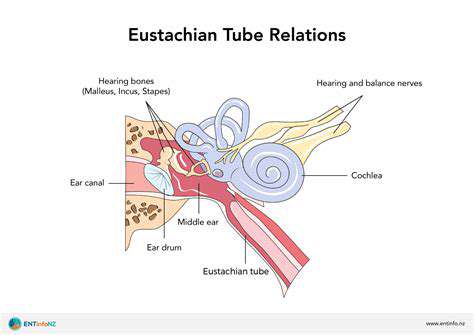
咽鼓管解剖與功能
咽鼓管咽
偏頭痛誘發因素及易感性
Read more about 飛機旅行壓力變化對偏頭痛的影響
原因、症狀與治療 了解颈部与后脑痛的常见原因,包括肌肉拉伤、颈椎问题及如鞭打伤等损伤。了解心理压力、医疗状况及生活方式因素如何影响不适。这本综合指南涵盖了值得关注的症状、有效的治疗方案,以及应采取的预防措施。探索改善姿势、定期运动及压力管理技巧的实用建议,以减轻疼痛并提高生活质量。识别何时应寻求医疗协助,并了解谘询医疗专业人员以获得适当诊断和量身定制治疗计划的重要性。不论您正经历急性疼痛或正在寻找长期的缓解策略,此资源提供了宝贵的见解以帮助您有效理解和管理颈部與後腦痛。
Oct 23, 2024
了解頭痛
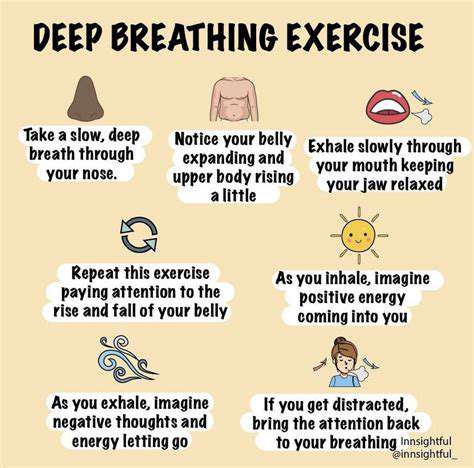
歡迎來到我們關於頭痛的綜合指南,我們將深入探討這一常見疾病的複雜性。了解原發性和繼發性頭痛之間的主要差異,包括偏頭痛、緊張型頭痛和叢集性頭痛等類型。探索可能加劇這些頭痛的常見誘因,從壓力和睡眠不足到飲食影響。了解針對特定頭痛類型的有效治療方案,從非處方藥物到生活方式調整和非藥物治療。我們的資源還強調何時尋求醫療幫助,並提供對較少見頭痛的見解,確保您能夠有效地管理症狀。保持了解最新的研究和個性化的方法,以幫助改善您的生活品質,使您能夠識別頭痛誘因並發現適合您的緩解策略。
Oct 31, 2024
了解咳嗽時肌肉拉傷的原因、症狀與緩解策略Meta描述:發現咳嗽引起的肌肉拉傷的原因、常見症狀和有效的緩解策略。學習如何預防和管理肌肉拉傷,以改善呼吸健康。---咳嗽時肌肉拉傷的原因是什麼?咳嗽是清理氣道的自然反射,但可能導致肌肉拉傷,特別是在胸部和腹部。本文探討了咳嗽時肌肉拉傷的機制、常見的加重因素以及整體肌肉健康的重要角色。咳嗽引起的肌肉拉傷的症狀學會識別像是局部疼痛、緊繃感和腫脹等症狀。理解這些跡象對於管理不適和預防慢性問題至關重要。預防措施和緩解策略探索預防咳嗽引起的肌肉拉傷的實用技巧,包括維持呼吸健康、補充水分和正確的呼吸技巧。發現有效的緩解方法,如熱冷療法、輕柔拉伸,以及何時尋求醫療建議。增強您的健康透過了解咳嗽與肌肉拉傷之間的關係,採取積極措施管理您的健康。與醫療專業人員諮詢,並參加鍛煉以增強您的肌肉抵抗力,從而改善健康。關於預防和管理咳嗽引起的肌肉拉傷的更多見解,請訪問我們的完整指南!
Dec 31, 2024
理解右側頭痛及其管理探索右側頭痛的常見誘因和症狀,包括緊張、飲食因素和環境影響。了解與這種疼痛相關的潛在醫學狀況,如偏頭痛和鼻竇感染,並學會何時尋求急診護理。我們的綜合指南概述了有效的管理策略,包括生活方式的改變、減壓技巧和醫療治療選擇。增強自己的知識,識別誘因並實施長期預防策略,以改善生活質量。訪問我們,深入了解右側頭痛的診斷和治療。
Jan 19, 2025