Accurate Diagnosis: The Key to Effective Medical Treatment
The Role of Proper Diagnosis in Patient Care
The Importance of Early Detection
Early detection of medical conditions is crucial for improving patient outcomes. Identifying health issues at an early stage allows for timely interventions that can save lives.
Health professionals often emphasize the need for regular screenings and check-ups to facilitate early diagnosis. This proactive approach can lead to more effective treatment options and better long-term health management.
Impact of Misdiagnosis
Misdiagnosis can have serious consequences, leading patients down the wrong treatment path. Inaccurate diagnoses can result in delayed treatment, worsening conditions, and increased healthcare costs.
It is essential for healthcare providers to utilize the best available diagnostic tools and methods to minimize the risk of errors. Continuous education and training are vital in helping practitioners stay updated on the latest developments in diagnostics.
Advancements in Diagnostic Technology
Recent advancements in medical technology have significantly improved diagnostic accuracy. Innovations such as artificial intelligence and advanced imaging techniques enable healthcare providers to detect conditions earlier than ever before.
These technologies not only enhance the precision of diagnoses but also reduce the time taken to identify ailments. As technology evolves, so too does the potential for more personalized and effective treatment plans.
Patient Involvement in Diagnosis
Engaging patients in the diagnostic process can lead to more accurate outcomes. When patients are informed about their symptoms and medical history, they can better communicate with their healthcare providers.
This collaborative effort fosters a stronger doctor-patient relationship and enhances the overall quality of care. Empowering patients to ask questions and voice concerns is essential for achieving accurate and timely diagnoses.
Challenges in Achieving Accurate Diagnoses
Factors Contributing to Diagnostic Errors
Diagnostic errors can arise from a variety of factors that affect the clinician's ability to make an accurate diagnosis. One major factor is the complexity of symptoms presented by patients, which can lead to misinterpretation. Symptoms that overlap among different conditions can create confusion, prompting incorrect assumptions.
Another significant contributor is related to the patient's history or the information they provide. Often, patients may not disclose all relevant information about their medical history, intentionally or unintentionally complicating the diagnostic process.
Additionally, the practice environment plays a crucial role. Time constraints in busy healthcare settings can lead to rushed evaluations, reducing the likelihood of thorough investigations or second opinions.
Communication breakdowns between healthcare providers also contribute to diagnostic errors. Inadequate handoffs between medical professionals can prevent critical information from being relayed, impacting patient outcomes.
Finally, reliance on technology can sometimes do more harm than good. While diagnostic tools can aid in assessments, over-dependence on them might discourage clinicians from using their clinical judgment.
Strategies to Enhance Diagnostic Accuracy
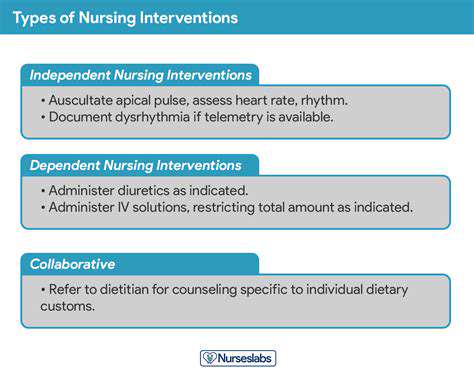
To improve diagnostic accuracy, healthcare systems must implement comprehensive training programs emphasizing the importance of thorough patient evaluations. Such training should include strategies for better communication with patients, enabling more detailed histories to be recorded.
Encouraging a culture of teamwork among healthcare providers is also beneficial. Collaboration can help to bring diverse perspectives, leading to more comprehensive evaluations and better diagnosis. Interdisciplinary meetings where medical professionals discuss complex cases could play a vital part in fostering such teamwork.
Additionally, investing in technologies that support rather than replace the human element in diagnostics is essential. For example, incorporating decision-support systems that assist clinicians in evaluating information rather than solely relying on them can help reduce errors.
Regular audits and feedback mechanisms can help identify recurrent patterns of errors within a practice or institution, leading to targeted improvements. This process not only enhances knowledge but also motivates practitioners to strive for higher standards.
Finally, patient involvement in their own care can significantly increase diagnostic accuracy. Empowering patients to ask questions and share their concerns enables healthcare providers to gather more information, ultimately leading to better outcomes.
Impact of Early Diagnosis on Treatment Outcomes
Understanding the Importance of Early Diagnosis
Early diagnosis plays a crucial role in managing and treating medical conditions. Identifying a disease in its initial stages often allows for a wider range of treatment options, which can greatly improve patient outcomes. Conditions such as cancer, diabetes, and heart disease can become severely more difficult to treat the longer they go undiagnosed.
When a diagnosis is made early, it enables healthcare providers to implement preventative measures and develop a treatment plan that is tailored specifically to the patient's needs. This personalized approach not only enhances the effectiveness of the treatment but also empowers patients, giving them a sense of control over their health journey.
Moreover, catching a disease early can significantly reduce the overall costs associated with treating advanced stages of illness. Effective management from the outset can prevent complications that typically arise from late-stage diagnoses, leading to fewer hospital admissions and less aggressive treatments.
Ultimately, the ability to detect health issues sooner rather than later can lead to improved survival rates and quality of life, making it clear why early diagnosis is essential in healthcare.
Barriers to Early Diagnosis
Despite the clear benefits, many patients face barriers that prevent early diagnosis. These can include a lack of access to healthcare resources, limited health literacy, and socioeconomic factors that hinder regular medical check-ups. Without proper access to health education and resources, individuals may not recognize the symptoms of potential health issues.
Cultural beliefs and stigmas can also play a significant role in delaying diagnosis. Some patients may hesitate to seek medical help due to fear, denial, or misconceptions about their health conditions. This can lead to deteriorating health and missed opportunities for effective intervention.
Additionally, healthcare system inefficiencies, such as long wait times for appointments or diagnostic tests, can contribute to delayed diagnosis. When patients cannot promptly access the care they need, it not only impacts individual health outcomes but also places a burden on the healthcare system as a whole.
Acknowledging and addressing these barriers is essential for improving the rate of early diagnoses and ensuring that more patients receive timely and effective care.
The Role of Technology in Improving Diagnosis
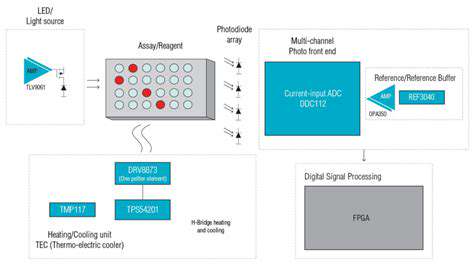
Advancements in medical technology have vastly improved the tools available for early diagnosis. Innovations such as telemedicine, AI-driven diagnostic tools, and advanced imaging techniques enable healthcare providers to diagnose conditions more accurately and quickly than ever before.
Telemedicine has expanded access to care, allowing patients to consult with their healthcare providers remotely. This can be particularly beneficial for those in rural or underserved areas who may otherwise struggle to receive timely medical attention.
Furthermore, artificial intelligence has shown great promise in the diagnostic field, with algorithms that can analyze medical images or data more efficiently than humans. These tools not only enhance the accuracy of diagnoses but also assist in identifying conditions that may be easily overlooked during traditional evaluations.
As technology continues to evolve, the potential for early and accurate diagnosis will only improve, leading to better treatment outcomes and enhanced patient care in the long run.
How Patients Can Advocate for Their Diagnostic Care
Understanding Your Rights as a Patient
Every patient has the right to understand their health conditions and the diagnostic processes involved. This knowledge is empowering and can help them make informed decisions about their care. Patients should be aware of their rights to ask questions, seek second opinions, and have a clear understanding of their treatment options.
Health care providers are obligated to provide clear and comprehensive information about diagnostic tests, including their purposes, potential risks, and what the results might mean. Patients should feel encouraged to engage in discussions about their care and to express any concerns they may have regarding their diagnoses.
Moreover, understanding insurance rights and coverage for diagnostic tests can play a crucial role in advocating for care. Patients should familiarize themselves with their insurance policies, as this knowledge can help them navigate any potential financial barriers to necessary tests.
Finally, patients should understand the processes available for filing complaints or grievances if they feel their rights have been violated, ensuring that their voices are heard in the healthcare system.
Effective Communication with Healthcare Providers
Clear and open communication is essential for effective advocacy in diagnostic care. Patients should practice articulating their symptoms and concerns in a manner that provides healthcare providers with a comprehensive understanding of their situation. Keeping a diary of symptoms can be helpful in communicating these details clearly.
Additionally, patients should ask for clarification on any medical jargon they do not understand. A good healthcare provider will appreciate the desire to better understand one's health and will be willing to explain concepts and terms that are not clear.
Taking a family member or friend to appointments can also enhance communication. They can help ask questions, take notes, and provide support, ensuring that the patient does not overlook important information or feel overwhelmed.
Furthermore, expressing preferences regarding care, such as the desire for minimal invasive procedures or holistic approaches, can also help tailor the diagnostic process to better meet individual needs.
Utilizing Resources to Enhance Advocacy
Patients can take advantage of various resources to enhance their advocacy efforts in medical diagnostics. Support groups play a crucial role by providing shared experiences and knowledge about specific illnesses or conditions, thus empowering patients with valuable insights and tips on navigating their care.
In addition, reputable online resources, such as health websites, medical journals, and patient advocacy organizations, can offer the latest information about symptoms, diagnostic tests, and treatment options. Patients should look for sources that are credible and backed by scientific research to ensure they are well-informed.
Healthcare professionals, such as nurses and social workers, can also provide guidance and support in understanding one's health situation and navigating the healthcare system. They can help empower patients to communicate their needs effectively.
Finally, maintaining a relationship with a primary care provider can offer continuity of care, which is essential for effective diagnostic assessments. They can advocate on behalf of patients, ensuring that their diagnostic care is thorough and meets their individual health needs.