Finding a Migraine Specialist: Tips for Choosing the Right Doctor
Resources like the American Migraine Foundation's provider database or university headache clinics often list specialists with proven track records. Local support groups can also provide unfiltered recommendations based on real patient experiences.
Considering Treatment Approaches and Therapies
Migraine management has evolved beyond painkillers. Today's options range from preventive medications to neuromodulation devices and even dietary interventions. When interviewing specialists, ask about their approach—do they favor medications first, or incorporate lifestyle modifications from the start?
Some clinics now offer multidisciplinary care with nutritionists and physical therapists. If alternative approaches like acupuncture interest you, seek providers who integrate these options responsibly rather than dismissing them outright.
Evaluating Communication Style and Comfort Level
The best medical expertise means little without good communication. During initial consultations, notice if the doctor asks about your lifestyle, listens without interrupting, and explains options clearly. Migraine management is often trial-and-error, so you need someone who partners with you through the process.
Red flags include dismissive attitudes (It's just stress) or one-size-fits-all treatment plans. Your ideal specialist should acknowledge migraine's complexity and customize their approach to your unique case.
Seeking Recommendations from Healthcare Professionals and Trusted Sources
Personal referrals often lead to the best matches. Ask your primary care physician which specialists their toughest migraine cases see. Pharmacists frequently know which doctors stay current on the latest treatments. Even online communities like migraine forums can reveal which local providers patients praise.
When receiving recommendations, ask specifically what impressed the referrer. Was it the doctor's diagnostic skills? Willingness to try new approaches? Bedside manner? These details help identify specialists whose strengths align with your priorities.
Researching Credentials and Specializations
Understanding Credential Types
In headache medicine, credentials tell part—but not all—of the story. Look for fellowship training in headache disorders specifically, not just general neurology. Certifications from organizations like the United Council for Neurologic Subspecialties indicate dedicated migraine expertise.
Some specialists pursue additional training in emerging areas like CGRP therapies or occipital nerve blocks. These focused qualifications can be particularly valuable for complex cases.
Evaluating the Validity of Credentials
With the rise of online certifications, verification matters. Cross-check credentials with state medical boards and specialty organizations. Beware of doctors claiming board certification from obscure organizations—legitimate certifications come from ABMS-recognized boards.
PubMed publications or conference presentations can further validate a specialist's expertise. Active researchers often bring cutting-edge approaches to their practice.
Investigating Specializations
Headache medicine has numerous subspecialties. Some neurologists focus on migraine prevention, while others specialize in refractory cases or pediatric headaches. If you experience vestibular migraines, for instance, you'd want someone versed in balance disorders.
Don't assume all headache specialists have equal training—some complete rigorous fellowships while others attend brief certification courses. Ask specifically about their training pathway.
Analyzing Experience and Practical Application
Beyond credentials, practical experience is telling. Ask potential specialists: What percentage of your practice focuses on migraine? and Do you treat many patients with symptoms like mine? Seasoned practitioners can often spot subtle patterns that less experienced doctors miss.
Patient testimonials—especially those describing similar cases to yours—can reveal how effectively a doctor translates knowledge into results.
Considering Relevance and Alignment
Ensure the specialist's expertise matches your specific needs. A doctor specializing in cluster headaches may not be ideal for someone with menstrual migraines. Review their published work or clinic website for clues about their focus areas.
If you've tried numerous treatments without success, seek specialists experienced in refractory cases rather than general headache management.
Evaluating Communication Style and Treatment Approach
Understanding Communication Styles
Effective migraine care requires clear dialogue. The best specialists explain complex concepts simply, without medical jargon. They should ask about your treatment goals—whether it's reducing attack frequency, minimizing medication use, or improving work performance.
Notice if they summarize your understanding periodically (So you're saying...)—this confirms they're truly listening and comprehending your experience.
Assessing Treatment Approach Philosophies
Migraine management philosophies vary widely. Some specialists prioritize preventive strategies, while others focus on acute rescue plans. The ideal approach often combines both, tailored to your specific pattern.
Ask about their stance on complementary therapies. Progressive specialists might incorporate mindfulness training or physical therapy alongside medications, while traditionalists may stick to pharmaceuticals alone.
Evaluating the Specialist's Knowledge Base and Experience
The migraine treatment landscape changes rapidly. Ask potential doctors how they stay current—through conferences, journal reviews, or research participation. Those involved in clinical trials often offer access to cutting-edge therapies.
Inquire about their experience with newer treatments like CGRP inhibitors or nerve blocks. Their response will reveal how proactively they update their practice.
Considering the Specialist's Availability and Accessibility
Migraines don't follow business hours. Learn the practice's policies for urgent concerns—do they offer same-day appointments for severe attacks? Telehealth options can be invaluable when in-person visits are impossible.
Ask about typical wait times for appointments and prescription refill processes. Complex approval processes for specialty medications can become significant barriers.
Considering Location, Availability, and Cost
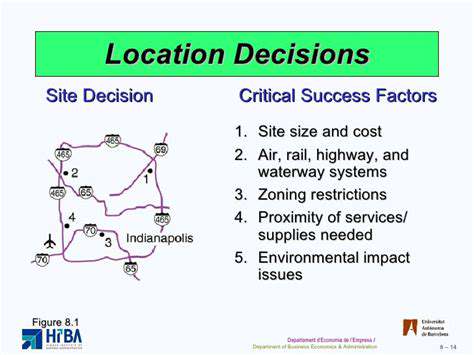
Location Considerations
While expertise matters, practicality counts too. Choose a specialist you can reasonably access during attacks. A world-renowned expert three hours away may be less helpful than a competent local provider.
Consider traffic patterns—a downtown clinic might be inaccessible during rush hour when migraines strike. Suburban or telehealth options sometimes offer more flexibility.
Availability of Resources
Specialized clinics often provide comprehensive services under one roof—neurologists, infusion centers, physical therapists. This integrated approach can streamline care compared to piecing together services separately.
Check if the facility has onsite imaging or lab services. Needing to visit multiple locations for diagnostics can delay treatment during flare-ups.
Insurance and Financial Factors
Migraine treatments range widely in cost. Verify which providers participate in your insurance network before committing. Some specialty medications require prior authorizations—ask how the practice handles these time-consuming processes.
If paying out-of-pocket, inquire about sliding scales or payment plans. Many clinics offer financial counselors to navigate coverage challenges.
Seeking Second Opinions if Needed

When to Consider a Second Opinion
Seeking another perspective makes sense when: Your current treatment isn't working, the diagnosis seems uncertain, or the proposed treatment carries significant risks. Complex cases often benefit from multidisciplinary review.
Don't worry about offending your doctor—competent specialists understand the value of second opinions and often encourage them for difficult cases.
Finding the Right Second Opinion
For second opinions, seek specialists at academic medical centers or headache specialty clinics. These providers often see more complex cases and have access to broader resources.
Prepare thoroughly—bring all prior test results, a detailed migraine diary, and a list of failed treatments. This helps the new specialist provide meaningful input rather than repeating previous assessments.
Integrating Multiple Perspectives
After receiving conflicting opinions, ask both doctors to explain their reasoning and discuss the discrepancies. Sometimes the truth lies between approaches—for instance, combining elements from both treatment plans.
Your primary care physician can often help mediate between specialists to develop a cohesive strategy.