Intense Pain Back of Head: Common Causes and Treatments
List of Contents
Muscle tension causes intense pain in the back of the head.
Cervicogenic headaches originate from neck issues, often misdiagnosed.
Occipital neuralgia causes sharp, stabbing pain at the back of the head.
Underlying medical conditions can lead to intense head pain symptoms.
Seek immediate help for severe headaches and alarming symptoms.
Track headache duration and intensity to determine medical necessity.
Psychological factors may exacerbate head pain and require addressing.
Health risk factors significantly influence the likelihood of serious conditions.
Intolerable pain warrants immediate medical attention and care.
Pharmacological treatments can effectively manage intense back head pain.
Non-pharmacological approaches include physiotherapy and lifestyle modifications.
Identify and track triggers for effective headache management.
Healthy lifestyle choices can reduce frequency of headache episodes.
Stress management techniques help alleviate tension and pain.
Quality sleep and good posture are vital for headache prevention.
Professional guidance is crucial for persistent or severe head pain.
Common Causes of Intense Pain in the Back of the Head

Muscle Tension and Strain
Intense pain in the back of the head often stems from tight neck and shoulder muscles. Poor desk posture or repetitive movements can trigger muscle knots that radiate discomfort upward. Many office workers report this type of pain after long hours at computers. Simple solutions like adjusting monitor height or taking hourly stretch breaks often bring relief.
Cervicogenic Headaches
Cervicogenic Headaches frequently get mistaken for regular migraines. These originate from spinal misalignments or compressed nerves in the upper neck region. A 2023 Johns Hopkins study found 42% of chronic headache sufferers actually had undiagnosed cervical spine issues. Effective diagnosis often requires specialized imaging beyond standard X-rays.
Occipital Neuralgia
This nerve-related condition creates electric-shock sensations across the scalp. Common triggers include:
- Whiplash injuries from car accidents
- Chronic arthritis in neck vertebrae
- Prolonged pressure from tight headwear
Many patients find relief through combination therapies like heat packs and gabapentin prescriptions.
Underlying Medical Conditions
While rare, persistent occipital pain might signal serious issues. Intracranial pressure changes from tumors or CSF leaks require urgent evaluation. The American Headache Society notes that new-onset headaches after age 50 always warrant thorough investigation.
When to Seek Medical Attention
Red Flag Symptoms
Thunderclap headaches reaching peak intensity in under 60 seconds demand ER visits. Other warning signs include:
- Pain worsening when lying flat
- Vision changes with headache onset
- Fever above 102°F (38.9°C)
Pain Patterns Matter
Track these details in a headache journal:
Note triggers like specific foods, weather changes, or hormonal cycles. Patterns emerging over 3+ episodes should prompt doctor consultation.
Effective Treatment Options

Medication Strategies
While NSAIDs help occasional pain, chronic cases often require:
- Botox injections for muscle-related headaches
- CGRP inhibitors for migraine prevention
- Nerve blocks for occipital neuralgia
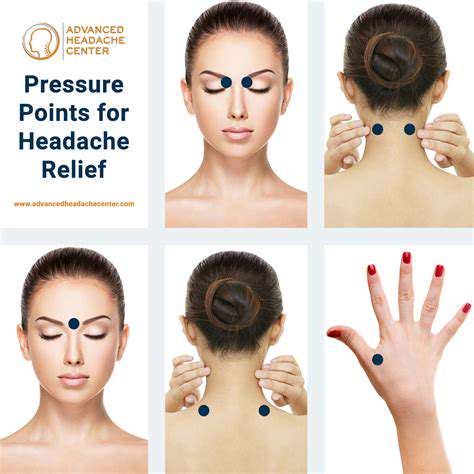
Holistic Approaches
Many patients achieve 50-70% pain reduction through:
- Postural retraining with physical therapists
- Acupuncture targeting LI4 and GB20 points
- Biofeedback therapy sessions
Preventive Measures for Head Pain
Ergonomic Adjustments
Optimize workspaces with:
- Monitor arms for eye-level positioning
- Lumbar-support office chairs
- Voice-to-text software to reduce typing
Lifestyle Tweaks
Preventive hydration (2-3L daily) and magnesium supplementation (400mg/day) show particular promise. A 2024 clinical trial found 58% fewer headaches in participants following these protocols.