Post Traumatic Headaches After Injury
Identifying Post-Traumatic Headaches: Common Symptoms
When someone suffers a head injury, they might later develop post-traumatic headaches (PH), a complication that frequently goes unrecognized. Spotting the wide array of symptoms early is vital for proper diagnosis and treatment. While many people report pounding pain, PH can show up in different forms, each disrupting daily routines in unique ways. Recognizing these subtle differences helps doctors tell PH apart from other headache types and choose the right treatment approach. Interestingly, the pain often starts slowly, sometimes appearing days or weeks after the initial injury, which makes early identification tricky. It's worth noting that the headache's intensity doesn't necessarily reflect how serious the original injury was.
Many patients describe an ongoing, mild ache concentrated in specific head areas. This discomfort might affect one side or both, radiating across the forehead, temples, or back of the skull. People often characterize the pain as pulsating, pressing, or sharp, with its strength changing throughout the day. Another telltale sign involves heightened reactions to light and sound, which can turn ordinary activities like reading or watching TV into challenging tasks. This increased sensitivity often serves as a crucial warning sign of PH and shouldn't be ignored.
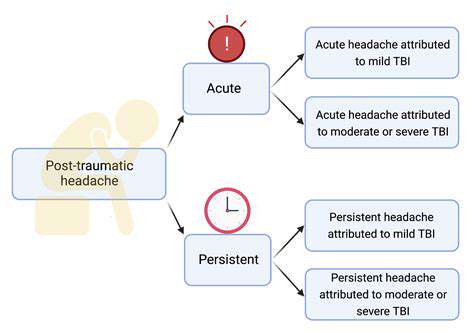
Variations in Post-Traumatic Headache Presentation
Post-traumatic headaches don't follow a standard pattern. How they appear depends on several factors including the injury's nature and severity, the person's existing health conditions, and whether other injuries occurred simultaneously. Some people might feel sudden, intense pain right after an incident, while others notice their usual headaches gradually worsening post-injury. Medical professionals need to understand these different patterns to make accurate diagnoses and create personalized treatment strategies. The pain level might also change during the day, sometimes intensifying with physical exertion or emotional stress.
Some patients experience nausea or vomiting alongside their headaches. This combination can be particularly troubling and requires prompt medical evaluation. Others might complain about neck stiffness or jaw pain, possibly linked to muscle tension or other health issues. These additional symptoms can make diagnosis more complex, emphasizing the need for doctors to carefully examine a patient's complete medical background.
Differentiating Post-Traumatic Headaches from Other Types
Distinguishing post-traumatic headaches from tension headaches or migraines presents a significant challenge since symptoms often overlap. The timing of headache onset relative to the injury and the presence of trauma-related symptoms often provide key clues. For example, a headache that starts right after a head injury more likely stems directly from that injury. A thorough medical evaluation becomes essential to eliminate other potential causes and determine the best treatment approach. Associated symptoms like memory lapses, thinking difficulties, or personality changes might also point to PH, though they don't always occur.
Doctors typically need a detailed medical history, physical examination, and sometimes imaging tests like MRI or CT scans to separate post-traumatic headaches from other conditions. The objective is to pinpoint the headache's exact cause and develop a customized treatment plan addressing the root problem. This differentiation process ensures patients receive care specifically suited to their condition.
Considering the patient's overall health and injury circumstances remains crucial. This comprehensive method helps healthcare providers make precise diagnoses and offer appropriate treatments tailored to each individual's needs.
Causes and Risk Factors for Post-Traumatic Headaches
Head Injuries and Their Aftermath
Post-traumatic headaches (PTH) commonly follow head injuries of any severity. Various injuries, ranging from minor concussions to serious skull fractures, can potentially trigger PTH. Understanding how these injuries occur—including impact forces, rotational forces, and affected brain areas—helps explain subsequent headache development. The initial impact's duration and intensity greatly affect whether headaches will develop and what form they might take.
The brain's complex system of nerves, blood vessels, and support structures can sustain damage during head trauma. Even slight impacts might cause microscopic tears and inflammation, setting off processes that lead to ongoing headache pain. Sometimes, the brain's natural healing mechanisms can unintentionally worsen the situation, creating long-term pain management issues.
Underlying Brain Structures and Their Role
Specific brain components like the meninges (protective brain membranes), blood vessels, and trigeminal nerve play pivotal roles in PTH development. Damage to these areas can cause inflammation, pressure changes, and altered nerve signaling—all contributing to headache pain. The exact location and extent of damage within these structures significantly influence the resulting headaches' type, frequency, and intensity.
Inflammation in the brain's support structures can trigger chemical reactions that send pain signals to the brain's pain centers. People's brains respond differently to this inflammation, leading to varied PTH experiences and treatment responses. Additionally, the brain's repair processes might sometimes contribute to continued discomfort.
Individual Predisposition and Factors
Personal factors can affect PTH likelihood and severity. Existing conditions like migraines, tension headaches, or previous head injuries might increase vulnerability. Stress levels, sleep quality, and general health can also influence how well the body recovers from head trauma, potentially affecting PTH development.
Genetic factors might determine how someone's body reacts to injury, with some people being naturally more prone to developing PTH. Lifestyle choices including diet, exercise, and hydration can impact healing and PTH potential.
Contributing Factors Beyond the Immediate Injury
While the initial injury plays the primary role, other elements can worsen or prolong PTH symptoms. These include stress, anxiety, and underlying medical conditions. Poor sleep, nutritional gaps, and dehydration can all hinder healing and pain management. The emotional impact of head injuries, including anxiety and depression, might indirectly prolong headaches.
Post-concussive syndrome—a group of symptoms following concussions—often features headaches prominently. The complex relationship between physical and psychological factors in post-concussive syndrome makes PTH management particularly difficult. Professional medical advice becomes essential for proper evaluation and customized treatment plans.

Dental sleep solutions operate through strategic anatomical adjustments - shifting jaw alignment and stabilizing tongue position to prevent airway blockages. This physical reconfiguration combats the tissue collapse responsible for 83% of obstructive apnea cases according to Sleep Foundation data. Patients frequently report improved breathing patterns within weeks of consistent use.