Supporting Teenagers Through Migraine Challenges
Recognizing the Unique Migraine Experience in Adolescence
Understanding the Diverse Presentation of Migraine
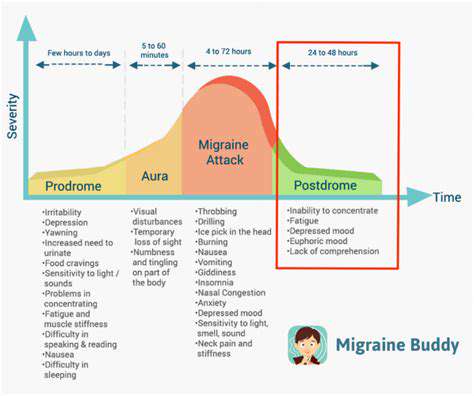
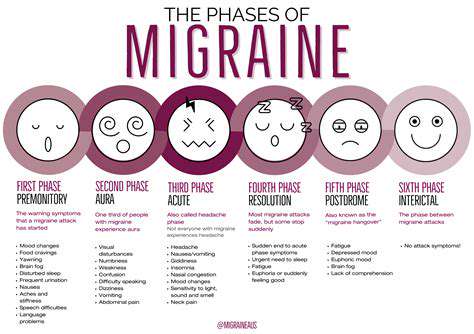
Migraine headaches represent far more than just severe headaches—they're a multifaceted neurological condition with symptoms that vary dramatically between individuals. The way migraines manifest can differ not just in pain intensity but also in accompanying symptoms and triggers. For some teens, visual disturbances or tingling sensations (aura) signal an impending attack, while others experience sudden nausea or light sensitivity without warning. This variability makes migraines particularly challenging to identify in adolescents, whose symptoms might be dismissed as stress or typical teenage complaints.
What's often overlooked is how migraine symptoms evolve during puberty. Hormonal changes can alter pain patterns, while academic pressures and irregular sleep schedules introduce new triggers. Recognizing these developmental nuances is crucial because adolescent migraines frequently differ from adult presentations in both duration and symptom quality. A headache that lasts forty minutes in a thirteen-year-old might be just as debilitating as a four-hour episode in an adult, yet often receives less medical attention.
Identifying Potential Triggers and Contributing Factors
The migraine trigger landscape shifts significantly during adolescence. While food sensitivities might trigger childhood migraines, teens often report stress from exams, social pressures, or screen time as predominant factors. Environmental elements like fluorescent classroom lighting or strong cafeteria smells become newly problematic. What makes adolescent triggers particularly tricky is their interaction with normal developmental changes—a growth spurt's nutritional demands might lower magnesium levels, while changing sleep needs disrupt circadian rhythms.
Emerging research suggests teenage brains process sensory input differently during migraine attacks. Loud noises that were tolerable at twelve might become unbearable at fifteen. This neurological hypersensitivity means triggers that were insignificant before puberty can suddenly become major precipitants, requiring constant reevaluation of what constitutes a true trigger versus normal adolescent experience.
Developing Effective Management Strategies
Migraine management in teens demands flexibility absent from adult protocols. Where adults might benefit from scheduled medications, adolescents often need school-friendly solutions—fast-acting abortives that don't cause drowsiness during exams, or discreet rescue medications for sleepovers. The most successful approaches combine medical interventions with lifestyle adaptations tailored to teenage realities, like hydration reminders synced to class bells or meditation apps disguised as games.
Prevention takes on new dimensions with adolescents. While adults might focus on medication compliance, teens often respond better to behavioral hacks—using blue-light filters during late-night studying, or strategic caffeine use before known trigger activities. Teaching self-advocacy skills proves particularly valuable, empowering teens to request lighting adjustments in classrooms or bathroom breaks when prodrome symptoms emerge.
Strategies for Effective Communication and Support
Active Listening and Empathy
When discussing migraines with teenagers, conventional listening often falls short. Their pain descriptions might be vague (my brain feels swollen) or expressed through behavior (withdrawing to a dark room). Effective listening requires decoding these non-traditional cues while resisting the urge to compare their experience to adult migraines. Validating statements like That sounds exhausting—how do you usually cope? often yield more insight than direct questioning.
Teens frequently describe migraine symptoms through metaphors that reflect their developmental stage. A fourteen-year-old might say It's like TikTok glitches in my vision while a seventeen-year-old compares it to a bad hangover without the party. Learning this metaphorical language helps clinicians and parents distinguish migraine patterns from other headaches while making teens feel understood.
Creating a Supportive Environment
School environments often unintentionally exacerbate adolescent migraines. Fluorescent lights that don't flicker visibly to adults may trigger photosensitivity in teens. Backpacks exceeding weight recommendations strain neck muscles. Simple modifications—permission to wear sunglasses indoors, access to quiet spaces, or leniency with assignment deadlines during recovery periods—can dramatically reduce migraine-related academic consequences.
Peer understanding remains a critical yet often neglected support element. Teens frequently report feeling judged when canceling plans last-minute or needing dark rooms during sleepovers. Educating friend groups about migraine realities—perhaps through social media content the teen approves—can transform social support networks into powerful allies in migraine management.
Open and Honest Dialogue
Migraine discussions with teens require balancing honesty with hope. While acknowledging migraine's chronic nature, emphasize the control they can develop through trigger identification and management techniques. Frame treatment plans as collaborative experiments rather than fixed regimens—Let's test if magnesium supplements help this month feels more engaging than Take these daily.
Technology often bridges communication gaps. Shared symptom-tracking apps allow teens to report discreetly while giving parents/clinicians real-time data. Messaging platforms enable check-ins that feel less intrusive than face-to-face questioning, especially for teens reluctant to discuss symptoms openly.
Identifying and Addressing Potential Triggers

Identifying Potential Issues
Trigger identification in adolescents requires detective work beyond standard checklists. A trigger journal should track not just food and sleep, but also social media use, academic pressures, and even posture during device use. Patterns often emerge across weeks—perhaps math tests consistently precede attacks, or weekend oversleeping triggers let-down migraines.
Emerging research suggests teenage migraine brains respond differently to stimuli than adult or child brains. Where adults might tolerate missing one meal, teens often need consistent protein intake to maintain blood sugar stability—making irregular eating patterns a uniquely potent adolescent trigger.
Assessing the Impact of Potential Issues
Not all triggers warrant equal attention. While perfume might cause brief discomfort, sleep deprivation could trigger multi-day attacks. Prioritization requires distinguishing between annoyances and true attack precipitants—a process best done collaboratively with the teen to ensure their lived experience guides the assessment.
Hormonal influences require special consideration in teens. Menstrual cycles often become regular just as academic pressures intensify, creating predictable yet unavoidable monthly trigger clusters. Recognizing these unavoidable patterns allows for strategic planning—scheduling lighter academic loads during predicted vulnerable periods, for example.
Developing Strategies to Mitigate Issues
Effective adolescent migraine strategies work within teenage lifestyles rather than against them. If late-night gaming can't be eliminated, suggest blue-light glasses and hydration breaks. For social media-addicted teens, gradual reduction strategies often succeed where cold-turkey approaches fail—perhaps limiting TikTok to 20-minute sessions with mandatory eye rests.
Peer-influenced triggers demand creative solutions. If cafeteria smells trigger attacks, packed lunches with strong mint gum might help. For concert-loving teens, specialized earplugs that reduce decibels without muffling music preserve social connections while minimizing risk.
Building a Support Network and Promoting Self-Care
Building a Strong Support System
Adolescent migraine support extends beyond medical professionals. Teachers who permit sunglasses, coaches who adjust practice intensities, and friends who understand cancellation policies all contribute to effective management. Creating a migraine ally network—people briefed on the teen's specific needs—reduces the isolation many young sufferers experience.
Online communities offer unique support opportunities. Moderated forums allow teens to connect with global peers facing similar challenges, often leading to innovative coping strategy exchanges. However, professional guidance helps navigate these spaces safely, ensuring advice aligns with medical recommendations.
Prioritizing Self-Care Strategies
Teen-friendly self-care differs markedly from adult approaches. Guided meditation might bore them, but biofeedback games could engage. Hydration reminders work better when tied to favorite apps, while sleep hygiene succeeds when framed as performance enhancement rather than health obligation.
Nutritional interventions require teenage realism. While kale smoothies might be rejected, protein-rich snacks compatible with backpack life often gain traction. The key is presenting self-care as empowerment tools rather than restrictions—This electrolyte mix might help you stay at the party longer versus You must drink this.
Understanding the Unique Challenges of Adolescent Migration
Migraine management during family relocation requires special consideration. New schools mean navigating unfamiliar trigger environments—different lighting, cafeteria smells, or stress patterns. Proactive strategies include pre-visiting new spaces to identify potential issues and establishing care continuity with new healthcare providers before crises arise.
Cultural factors compound relocation challenges. Some cultures stigmatize chronic pain, while others have traditional remedies that may complement or conflict with medical advice. Respecting these beliefs while ensuring safe care requires sensitive, individualized approaches.