Vestibular Migraines: Managing Dizziness and Vertigo
List of Contents
Vestibular migraines cause dizziness, vertigo, and balance issues.
Triggers include stress, certain foods, and sleep irregularities.
Effective management combines lifestyle changes and medications.
Cognitive-behavioral therapy helps with chronic migraine-related anxiety.
Maintaining diaries aids in identifying symptoms and triggers.
Acupuncture and nutritional changes may alleviate symptoms.
Severe symptoms require immediate medical attention and assessment.
What Are Vestibular Migraines?

Understanding the Mechanism Behind Vestibular Migraines
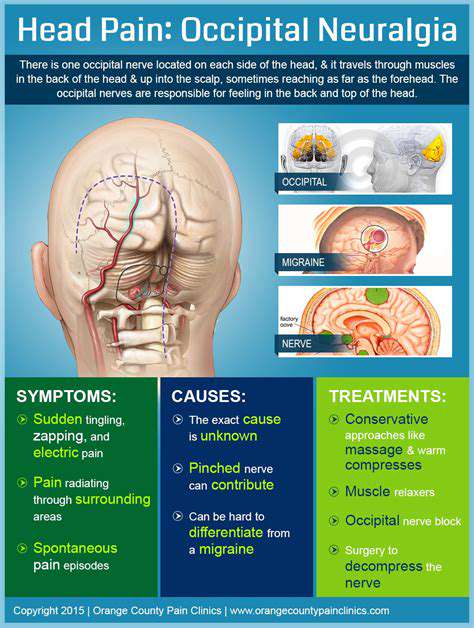
Vestibular migraines, often characterized by sensations of dizziness or vertigo, stem from complex interactions within the vestibular system. This system helps maintain balance and spatial orientation when we move. Research indicates that individuals experiencing vestibular migraines may have an altered sensitivity to sensory stimuli, leading to the perception of motion without actual movement.
The migraines themselves can be triggered by various factors, including stress, lack of sleep, and certain foods. A study published in the Journal of Neurology highlighted the correlation between migraine frequency and vestibular dysfunction, underscoring the need for comprehensive evaluations of patients with recurrent dizziness. Understanding these underlying mechanisms helps pave the way for tailored prevention strategies.
Effective Management Strategies for Vestibular Migraines
Managing vestibular migraines requires a multi-faceted approach that combines lifestyle modifications and medical interventions. Engaging in regular physical activity, maintaining a consistent sleep schedule, and avoiding known triggers can significantly impact frequency and severity. For many, keeping a headache diary to identify patterns and triggers is invaluable.
- Avoid common food triggers such as aged cheese, alcohol, and caffeine.
- Incorporate relaxation techniques such as yoga or meditation to reduce stress.
- Consult with a healthcare professional about potential medications that can help prevent migraines.
On the medical side, treatments often include preventive medications like beta-blockers or anticonvulsants. It's essential for individuals to work closely with neurologists or headache specialists to find the right regimen tailored to their symptoms. Additionally, cognitive-behavioral therapy has shown promising results in helping patients cope with the psychological aspects of chronic dizziness and anxiety related to migraines.
Identifying Symptoms and Triggers
Understanding the Symptoms of Vestibular Migraines
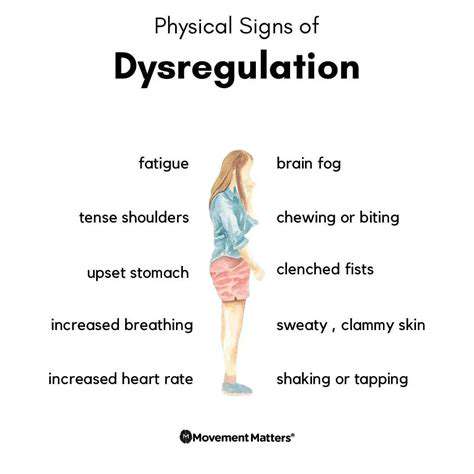
Vestibular Migraines can present with a variety of symptoms that differ from typical migraine headaches. Patients often experience episodes of dizziness or vertigo, which can last from several minutes to several days. Additionally, many report symptoms such as imbalance, nausea, and even motion sensitivity, making everyday activities challenging.
Besides the vestibular symptoms, individuals may also experience aura, which can manifest as visual disturbances. These disturbances can include zigzag patterns, flashes of light, or blind spots, providing a multifaceted challenge when diagnosing these migraines. Understanding these symptoms is crucial for effective management and treatment.
Common Triggers of Vestibular Migraines
Identifying triggers is vital for managing vestibular migraines. Some common triggers include specific foods, stress, hormonal fluctuations, and changes in sleep patterns. For instance, aged cheeses, red wine, and processed meats can be dietary culprits that provoke episodes for some individuals.
Stress, both physical and emotional, is another significant trigger. Stress management techniques such as mindfulness and yoga can be beneficial in reducing the frequency of migraine episodes. Tracking these triggers can help patients gain insights into their specific patterns and develop a more tailored management plan.
Environmental triggers are also noteworthy. Bright lights, strong odors, and unexpected movements can trigger vestibular migraines in susceptible individuals. Keeping a detailed diary of situations that precede an episode can help identify personal triggers more accurately.
The Role of Lifestyle in Managing Symptoms
Lifestyle changes play a vital role in managing the Symptoms of vestibular migraines. Regular exercise can improve overall balance and reduce stress levels, which, in turn, might help decrease the frequency of migraine attacks. Activities like walking, swimming, or cycling, tailored to one’s ability, can promote a healthier lifestyle.
Maintaining a consistent sleep schedule is another essential aspect. Sleep deprivation or irregular sleep patterns can act as significant triggers. Establishing a routine can help enhance sleep quality and length, thereby reducing the likelihood of experiencing vestibular migraine symptoms.
Seeking Professional Help for Diagnosis
Recognizing the need for professional evaluation is crucial for individuals experiencing recurrent vestibular symptoms. A healthcare provider can conduct a thorough assessment, including a detailed medical history and, if necessary, imaging tests to rule out other conditions. Accurate diagnosis is important to direct appropriate treatment and management options.
Treatment Options for Vestibular Migraines
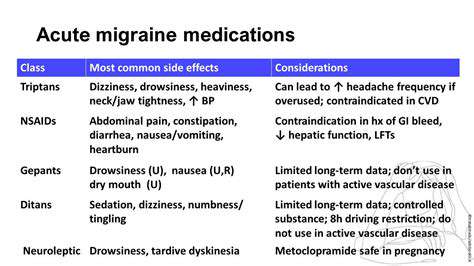
Treatment for vestibular migraines often requires a multi-faceted approach. Medications can range from over-the-counter pain relievers to prescription drugs like triptans or preventative medications such as beta-blockers and anticonvulsants. The choice of medication largely depends on individual response and frequency of episodes, emphasizing the importance of personalized treatment plans.
In addition to medication, lifestyle modifications and alternative therapies, such as vestibular rehabilitation therapy (VRT), can be helpful. VRT focuses on exercises to improve balance and reduce dizziness; many patients find it beneficial in conjunction with other treatments.
The Importance of Monitoring and Reporting Symptoms
Keeping a detailed symptom diary can significantly enhance the ability to manage vestibular migraines. Note the timing, duration, and intensity of symptoms, as well as any associated triggers or mitigating factors. This information can be invaluable during consultations with healthcare professionals, allowing for more informed treatment decisions.
Patients are encouraged to openly communicate with their healthcare providers about their symptoms and how frequently they occur. Such discussions can lead to more tailored treatment strategies and provide insight into effective coping mechanisms.
Effective Treatment Options
Pharmacological Interventions
Several medications have shown effectiveness in managing vestibular migraines. Triptans, commonly used to treat acute migraines, can also provide symptomatic relief for individuals experiencing vestibular symptoms. A study published in the ‘Headache’ journal found that triptans significantly reduced the severity and frequency of vestibular symptoms in participants diagnosed with vestibular migraines.
Another class of medications, including beta-blockers and anticonvulsants, may help in both preventive and acute phases. Propranolol, a beta-blocker, has been notably effective for many patients. According to various clinical guidelines, initiating a low dose and gradually adjusting it may yield better results while minimizing side effects.
Non-Pharmacological Strategies
In addition to medical therapies, non-pharmacological strategies are crucial for managing vestibular migraines effectively. Vestibular rehabilitation therapy (VRT) has gained recognition for alleviating balance issues and dizziness. Tailored exercises can help improve strength and coordination, which in turn can lessen the episodes of vertigo. Evidence from the ‘Journal of Vestibular Research’ suggests that VRT not only enhances physical balance but can also positively impact psychological well-being by reducing the fear associated with vertiginous episodes.
Dietary modifications can also play a role in managing vestibular migraines. Many patients report that triggering foods, such as aged cheeses and processed meats, often exacerbate their symptoms. Keeping a detailed food diary can help identify specific triggers, allowing individuals to adjust their diets accordingly. Furthermore, hydration and regular meal schedules may reduce the frequency of migraine attacks.
Lastly, Mindfulness and Stress-reduction techniques, such as yoga and meditation, have been shown to benefit migraineurs. A review in 'The Journal of Alternative and Complementary Medicine' indicated that practices promoting relaxation can help minimize stress-induced triggers leading to vestibular migraines.
The Role of Alternative Therapies

Understanding Vestibular Migraines
Vestibular migraines are a type of migraine that primarily impacts balance and spatial orientation. They can present symptoms like dizziness, vertigo, and imbalance, often even in the absence of a headache. According to the American Migraine Foundation, approximately 40% of people with migraines experience some vestibular symptoms. This condition can greatly disrupt daily activities and may lead to significant lifestyle changes.
Mechanisms Behind Alternative Therapies
Alternative therapies often target the neurological pathways and muscle tension that may contribute to vestibular migraine symptoms. These treatments can include acupuncture, herbal medicine, and various forms of physical therapy. Recent studies show that techniques like vestibular rehabilitation can improve balance and reduce dizziness, promoting a better quality of life for sufferers.
Understanding the body’s response to these therapies involves exploring the connection between stress, tension, and migraines. Research by the National Institutes of Health indicates that mind-body techniques can significantly diminish the frequency and intensity of migraine episodes. By addressing underlying issues like anxiety and muscle tension, patients may find additional relief.
Acupuncture as a Therapeutic Option
Acupuncture involves inserting thin needles at specific points in the body to balance energy flow, known as Qi. Studies have shown that acupuncture can reduce both the frequency and severity of migraines, including vestibular types. A clinical trial published in the journal Headache found that patients receiving acupuncture reported a 50% reduction in their migraine days per month.
It's essential for individuals considering this therapy to seek treatment from certified practitioners who specialize in managing migraines. Tracking symptoms before and after sessions can provide useful insights into the effectiveness of acupuncture for personal cases.
Nutritional Interventions
- Eating a balanced diet can help manage migraine triggers.
- Supplements like magnesium and riboflavin have shown efficacy.
- Staying hydrated is crucial for reducing migraine frequency.
Certain dietary changes may also play a pivotal role in alleviating vestibular migraine symptoms. Incorporating foods rich in magnesium, such as nuts and leafy greens, can help prevent migraines. Additionally, riboflavin (vitamin B2) is backed by research indicating a significant decrease in migraine frequency when taken at high doses daily.
Moreover, maintaining hydration is often underestimated in its effectiveness. Dehydration can act as a migraine trigger, so ensuring fluid intake is vital for those prone to vestibular migraines.
Mindfulness and Stress Management
Mindfulness practices, including yoga and meditation, can effectively manage stress levels. Chronic stress is a known trigger for many migraine sufferers. A study published in the journal Neurology demonstrated that patients engaging in regular mindfulness exercises experienced fewer migraines and improved overall well-being.
The implementation of stress-reduction techniques can be simple and require minimal investment, making it accessible for most individuals. Simple breathing exercises, coupled with guided imagery, can also have profound effects in reducing tension and promoting a sense of calm.
Consulting with Healthcare Professionals
It’s vital for patients experiencing vestibular migraines to consult healthcare professionals before embarking on any alternative therapies. Neurologists or specialists in headache medicine can provide insight into the safest and most effective treatment options tailored to individual needs. Ongoing communication between patients and doctors can facilitate an integrated approach to managing migraines.
Regular follow-ups and monitoring will help ensure that the chosen alternative therapies align well with traditional treatments. This combined approach can help patients achieve better control over their symptoms, leading to a more manageable lifestyle.
When to Seek Medical Advice
Identifying Severe Symptoms
When dealing with vestibular migraines, it's crucial to recognize when symptoms escalate beyond typical discomfort. Severe Symptoms can include prolonged dizziness that hinders daily activities and persistent headaches. If dizziness lasts more than 72 hours or if headaches become debilitating, immediate medical attention is warranted. Both persistent symptoms and their severity can signal the need for a thorough examination to rule out other potential conditions.
Moreover, any sudden changes in symptoms, such as the development of hearing loss or changes in vision, should raise alarm bells. It's important to be vigilant — these changes might indicate complications or additional underlying issues. Consulting a healthcare professional for detailed evaluations, such as an MRI, can provide clarity and ensure appropriate treatment methods are employed.
Triggers That Require Prompt Intervention
Certain triggers can suggest a heightened risk for individuals suffering from vestibular migraines. For instance, frequent exposure to specific aromas or foods known to trigger migraines can lead to greater frequency or intensity of episodes. Keeping a detailed diary of these triggers may be beneficial for both patients and practitioners in identifying patterns that point to necessary lifestyle adjustments or medical interventions.
In addition, if a migraine occurs after engaging in activities like significant physical exertion or sudden changes in head position, this could indicate a need for immediate medical review. Engaging in preventive measures, such as managing stress or avoiding known triggers, can dramatically reduce the number of episodes experienced. Consulting a healthcare provider about preventive medication can also be a proactive step towards managing vestibular migraines effectively.