Why Assessing Severity is Crucial for Effective Treatment Outcomes
The Link Between Severity Assessment and Treatment Choices
The Importance of Accurate Severity Assessment
Accurate assessment of severity is a critical component in determining the appropriate treatment plan for patients. An accurate understanding of the severity can significantly impact patient outcomes. Clinicians must utilize standardized tools and methods to evaluate the severity patiently. The nuances in severity levels can indicate varying degrees of intervention that may be required. Without proper assessment, there is a risk of either under-treatment or over-treatment, leading to potential complications for the patient.
The type of diagnosis often correlates directly with the severity. For instance, a severe case of a condition may require immediate and aggressive treatment. Conversely, a mild case may only need monitoring or less invasive interventions. Thus, early and accurate assessment is fundamental to effective care. This information not only aids in clinical decision-making but also guides future treatment adjustments based on the patient’s response.
Additionally, accurate severity assessments can enhance communication among healthcare professionals. When every member of the care team understands the severity level, collaborating on treatment becomes more streamlined. This cohesive understanding helps in effectively utilizing resources and ensuring that every aspect of the patient's care is straightforward and coordinated.
Impact on Patient Compliance and Satisfaction
Understanding the severity of a condition can significantly influence a patient’s willingness to comply with treatment recommendations. Patients are more likely to follow through with treatment if they grasp the seriousness of their condition. When patients see a clear rationale for the proposed interventions, their satisfaction and engagement increase. This connection ultimately fosters better outcomes and helps maintain long-term health benefits.
Furthermore, discussing severity with patients opens the door for shared decision-making. This process allows patients to express their concerns and preferences, creating a collaborative environment in which they feel valued and understood. Patient engagement becomes a key component when they are informed about why certain treatments are necessary based on severity.
As a result, improved patient compliance not only fosters better health outcomes but also enhances the patient-provider relationship. When patients feel respected and involved, their trust in the healthcare system solidifies. Maintaining open lines of communication regarding severity encourages ongoing dialogue and provides a solid foundation for future healthcare encounters.
Tailoring Treatment Based on Severity Levels
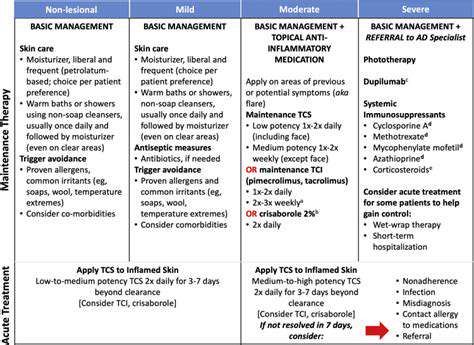
Different severity levels often dictate the type and intensity of treatment options available. For example, a patient experiencing mild symptoms may only require lifestyle modifications, whereas someone with moderate to severe symptoms might need a combination of medication and therapy. By accurately categorizing severity, clinicians can tailor interventions specifically suited to individual needs. Such customization can lead to more effective therapies and a reduction in unnecessary side effects.
Moreover, treatment plans can be adjusted based on ongoing severity assessments. Regularly evaluating a patient’s condition allows for timely alterations in care, ensuring that the treatment remains effective. If a patient's condition worsens, the increase in severity necessitates a reassessment, prompting immediate adjustments in therapeutics.
By tailoring treatment based on severity, healthcare providers can maximize their resources and focus on interventions likely to yield positive results. This approach not only optimizes clinical outcomes but also improves healthcare efficiency across the board, benefiting both practitioners and patients alike.
Improved Patient Outcomes from Timely Intervention
Understanding the Impact of Severity Assessment
Assessing the severity of a patient's condition is fundamental to tailoring effective treatment plans. By determining how severe a condition is, healthcare providers can prioritize interventions that are most critical to the patient's health.
Moreover, severity assessments guide clinical decision-making, ensuring that resources are allocated efficiently and effectively. This helps avoid unnecessary treatments that may not yield significant benefits for the patient.
With a clear understanding of the severity, healthcare teams can set realistic goals and expectations for both the patient and their families, fostering a cooperative environment.
Additionally, accurate severity assessments can help reduce the likelihood of complications, as timely interventions can mitigate risks associated with advanced disease progression.
Ultimately, assessing severity creates a foundation for continuous monitoring and adjustment of treatment strategies, enhancing the overall quality of care provided to patients.
The Role of Early Detection in Treatment Efficacy
Early detection of symptoms and timely severity assessments significantly affect treatment efficacy. When conditions are identified early, healthcare providers can intervene before the disease progresses to a more severe state.
Programs that emphasize routine screenings and assessments often lead to early diagnosis, allowing for a better prognosis and shorter recovery times. This early approach can ultimately decrease healthcare costs by minimizing the need for more extensive treatments.
In many cases, early intervention can transform the trajectory of illnesses such as cancer and heart disease, where outcomes are closely linked to the stage at which treatment begins.
Furthermore, educating patients about the importance of recognizing symptoms and seeking help early enriches their engagement in the treatment process and enhances overall health management.
By prioritizing early detection, healthcare systems can shift from reactive to proactive care, improving quality of life for countless patients.
Integrating Patient-Centered Approaches with Severity Assessments
Integrating patient-centered approaches in severity assessment ensures that treatment planning aligns with patients' individual needs and preferences. Engaging patients in discussions about their conditions can lead to more meaningful assessments of severity from both clinical and personal perspectives.
When patients feel involved in their care, they are more likely to adhere to treatment plans and follow medical advice, thereby improving outcomes.
Utilizing tools such as shared decision-making models helps patients express their values and concerns, fostering a partnership between patients and providers in navigating treatment options.
Moreover, understanding the psychological and emotional impact of severity can aid healthcare teams in providing comprehensive support, addressing issues such as anxiety or depression, which may influence treatment effectiveness.
Ultimately, integrating patient-centered approaches with severity assessments not only elevates the quality of care but also promotes a holistic understanding of health, leading to better long-term outcomes.
Holistic Care Through Severity Assessment
Understanding the Impact of Severity Assessment
Severity assessment plays a fundamental role in healthcare decision-making. By accurately measuring the intensity of a patient's condition, healthcare providers can tailor treatment plans that are both effective and efficient. This individualized approach ensures resources are allocated appropriately, reducing unnecessary interventions and focusing on what truly matters for the patient's health.
Moreover, understanding severity helps in predicting potential complications that may arise during treatment. For example, patients with higher severity levels may require more aggressive monitoring and intervention strategies. This foresight allows for proactive management, potentially improving overall outcomes.
Finally, severity assessment enhances communication among healthcare teams. When each member understands the severity of a patient's condition, collaboration becomes more streamlined, and treatment strategies can be aligned. This shared understanding fosters a comprehensive approach that supports better health outcomes.
Integrating Severity Assessment in Treatment Plans
Integrating severity assessment into treatment plans is essential for optimizing patient care. It informs clinicians about the appropriate frequency and intensity of treatments. For instance, patients with mild conditions may benefit from outpatient care, while those with severe presentations might require hospitalization and immediate interventions.
Additionally, severity assessments allow healthcare teams to prioritize cases based on urgency. By categorizing patients according to their severity levels, medical staff can efficiently manage their workload, ensuring that critical cases receive immediate attention. This prioritization can be the difference between life and death in some situations.
Incorporating severity assessments also encourages periodic re-evaluation of the treatment plan. As patient conditions evolve, ongoing assessments ensure that treatment methods remain suitable, allowing for timely adjustments that can enhance recovery times and overall health outcomes.
The Role of Technology in Severity Assessment
Advancements in technology have revolutionized the approach to severity assessment, providing healthcare professionals with tools that enhance accuracy and expediency. Electronic health records (EHR) and clinical decision support systems can aggregate patient data, allowing for real-time analysis of severity parameters. This integration leads to faster and more precise treatment decisions.
Moreover, emerging technologies, such as artificial intelligence and machine learning, are being utilized to predict severity outcomes based on historical data. Such predictive analytics enable clinicians to anticipate the potential trajectory of a condition, offering insights that can significantly influence treatment strategies.
Telemedicine also plays a crucial role in severity assessment by extending reach to patients in remote areas. Through virtual consultations, healthcare providers can assess symptoms and severity without the need for physical visits, fostering timely intervention and continuous monitoring of patients who may lack access to traditional healthcare facilities.
The Patient Perspective on Severity Assessment
From the patient's viewpoint, understanding severity assessment is vital for personal empowerment in their healthcare journey. When patients are informed about the severity of their condition, they can engage more effectively in their treatment plans. This knowledge helps them comprehend the necessity for specific procedures and follow-up appointments.
Furthermore, patients who are aware of their severity levels can communicate more openly with their healthcare providers. This transparency fosters a collaborative environment where patients feel valued and understood, ultimately enhancing trust between them and their medical team.
Finally, as patients participate in the severity assessment process, they can take proactive steps in managing their health. This involvement may include lifestyle adjustments, adherence to medication, and recognizing when to seek further medical attention—skills that are invaluable for long-term wellness.

