Explore comprehensive insights into migraines and headaches including causes, triggers, treatments, and natural remedies. Empower yourself with knowledge to manage pain effectively and improve your daily well-being
Essential Oils for Headache Relief: Peppermint, Lavender, and More
Jul 11, 2025
Coenzyme Q10 (CoQ10) and Migraines: Exploring the Link
Jul 11, 2025
Stress and Headaches: Managing the Number One Trigger
Jul 10, 2025
Integrating Mind Body Practices into Your Migraine Care Plan
Jul 10, 2025
Effective Pain Management Strategies You Can Control
Jul 10, 2025
Managing Migraine Triggers in Shared Living Spaces
Jul 10, 2025
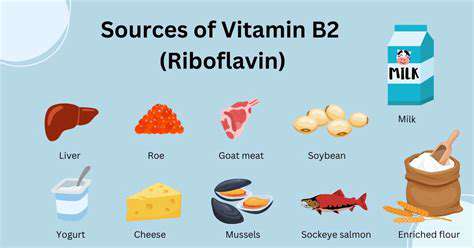
The Benefits of Riboflavin (Vitamin B2) for Migraine Prevention
Jul 09, 2025
Sinus Headache or Migraine? How to Tell the Difference
Jul 09, 2025
Understanding Silent Migraines: Symptoms Without the Pain
Jul 09, 2025
Accessing New Migraine Treatments: Insurance and Costs
Jul 09, 2025
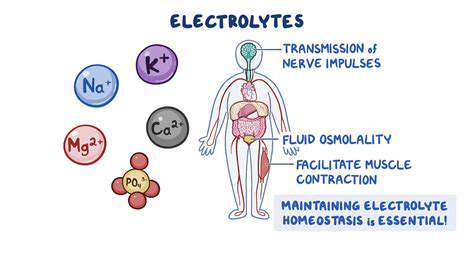
The Role of Potassium and Sodium Balance in Migraine
Jul 09, 2025
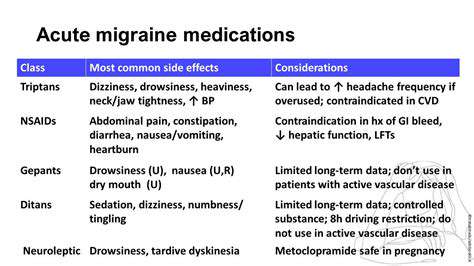
Combining Acute and Preventive Migraine Therapies
Jul 08, 2025
Barometric Pressure Headaches: Fact or Fiction?
Jul 08, 2025
The Difference Between Episodic and Chronic Migraine
Jul 08, 2025
OTC Pain Relievers: Ibuprofen vs. Acetaminophen vs. Naproxen for Headaches
Jul 07, 2025
Creating a Migraine Action Plan for Attack Days
Jul 07, 2025
Planning Ahead: Strategies for Migraine Prevention
Jul 07, 2025
Over the Counter Headache Relief: Choosing the Right Option
Jul 06, 2025
Natural vs. Medical Migraine Treatments: Pros and Cons
Jul 06, 2025
Reading Food Labels to Avoid Hidden Migraine Triggers
Jul 06, 2025