Understanding the Complexity of Migraines
Migraines are not just severe headaches; they are a complex neurological condition with varying symptoms and triggers. Characterized by intense, often debilitating pain, migraines can also involve nausea, sensitivity to light, and even visual disturbances. Research indicates that approximately 12% of the population suffers from migraines, highlighting the condition's prevalence and impact.
It's estimated that women are three times more likely to experience migraines compared to men, which suggests hormonal factors play a significant role in the condition. This complexity means migraines require a nuanced understanding that goes beyond merely labeling them as 'bad headaches.'
The Neurological Basis of Migraines
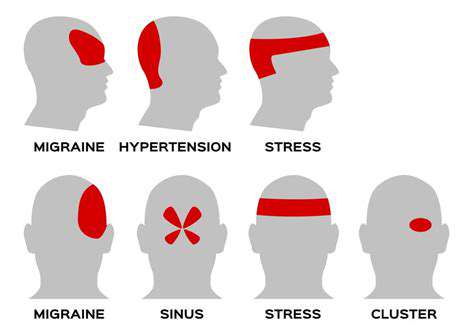
The pathophysiology of migraines is intricate, involving various pathways in the brain. An imbalance in neurotransmitters, including serotonin, has been implicated in Migraine Attacks. The International Headache Society categorizes migraines based on specific criteria that doctors use to differentiate them from other types of headaches, affirming their unique nature.
Furthermore, new research has revealed the role of cortical spreading depression, a phenomenon that likely contributes to the aura some migraine sufferers experience. This underscores that migraines are not simply an inconvenience but a serious medical condition with well-defined neurological underpinnings.
For those managing migraines, it's essential to recognize that effective treatment often involves more than just pain relief; preventive strategies targeting lifestyle changes and medication management are pivotal.
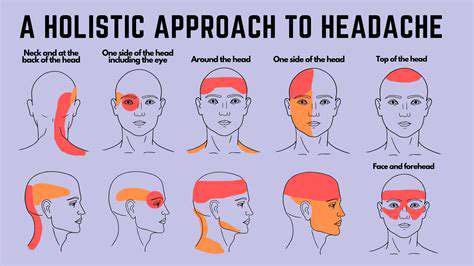
Identifying Triggers and Symptoms
Unlike typical headaches, migraines often come with a series of identifiable triggers. Common triggers include stress, certain foods, hormonal changes, and environmental factors. Keeping a migraine diary can significantly aid patients in pinpointing these triggers, leading to better management of their condition.
The aura associated with some migraines can serve as a warning sign, allowing individuals to prepare for an impending attack. Symptoms can vary greatly, and in some cases, they may present differently between individuals, which complicates the diagnostic process.
The Importance of Accurate Diagnosis
Mislabeling migraines as simple headaches can lead to inadequate treatment and management strategies. A thorough diagnosis by a healthcare professional is crucial for establishing an effective treatment plan. Neurologists often utilize specific criteria and tools to differentiate between migraines and other headache disorders.
It’s vital for patients to advocate for themselves and seek comprehensive evaluations, especially if they are experiencing migraine-like symptoms. With advancements in understanding the condition, there's a growing array of treatment options available, ensuring that those affected can find relief and regain control of their lives.
Myth 2: Only Adults Get Migraines

Understanding Migraines in Children and Teens
While many people associate migraines solely with adults, research indicates that children and teenagers can also suffer from these debilitating headaches. In fact, studies show that about 10% of children experience migraines, and the prevalence increases with age. In some cases, children may experience symptoms such as nausea, vomiting, and sensitivity to light, similar to adults. This indicates that developmental changes do not necessarily limit the impact of migraines.
It's crucial for caregivers to recognize migraine symptoms in young individuals. Frequent headaches that interfere with school or social activities should not be dismissed as normal. Understanding the signs can lead to timely interventions and treatment, ultimately improving the quality of life for affected children.
Debunking the Myths Surrounding Pediatric Migraines
- Children can experience migraines just like adults.
- Migraine triggers vary significantly across age groups.
- Pediatric migraines may present differently than in adults.
- Early diagnosis can lead to more effective management strategies.
It's important to note that myths surrounding Pediatric Migraines can prevent effective treatment. Many believe that migraines are infrequent in children; however, research shows a strong genetic component affecting children similarly to adults. Ignoring these early signs can lead to chronic migraines in adulthood, making early diagnosis essential. Migraines can manifest with unique triggers in children, such as dietary changes or stress from school, which differ from adult triggers.
Strategies for Managing Migraines in Younger Populations
Managing migraines in children and teens requires a tailored approach that differs from adult treatments. Pediatric patients often respond better to non-pharmaceutical interventions first, such as lifestyle adjustments and behavioral therapies. Techniques like biofeedback and cognitive-behavioral therapy have shown promise, particularly in children who may be hesitant about medication.
In addition to psychotherapy, dietary modification is also crucial. A balanced diet that avoids known triggers, such as processed foods, chocolate, or excessive caffeine, can help mitigate migraine occurrences. Children should be educated about their condition, encouraging them to keep headache diaries to identify patterns or triggers.
Myth 3: Migraines Are Triggered Only by Food
Common Food Triggers: What You Need to Know
While certain foods can indeed provoke migraines, research shows they're just one part of a complex puzzle. Common culprits like aged cheese, processed meats, and fermented foods can trigger headaches in some individuals. However, for many, these foods are not the primary instigators. Interestingly, a study highlighted in the Journal of Headache and Pain found that while 32% of patients reported food as a trigger, environmental factors played a more significant role in their migraines.
Moreover, the relationship between food and migraines is highly individual. What triggers a headache for one person may not affect another at all. Keeping a headache diary can help pinpoint your unique triggers, giving you a clearer understanding of your specific situation. By identifying patterns, individuals can make informed decisions about dietary choices without eliminating entire food groups unnecessarily.
Other Environmental Triggers of Migraines
Migraines can often be triggered by environmental factors such as changes in weather, exposure to bright or flickering lights, and strong odors. A significant number of migraine sufferers report that thunderstorms and changes in air pressure lead to migraine episodes. This suggests that environmental conditions might often surpass dietary influences in triggering headaches.
Moreover, stress is another major environmental trigger associated with migraines. Studies indicate that emotional stress is linked to the onset of headaches and can even prolong the migraine experience. Therefore, while food is a noteworthy aspect to consider, evaluating stress levels, surroundings, and even sleep patterns can unveil other triggers that may be far more impactful.
The Role of Hormones in Migraine Triggers
Hormonal fluctuations, particularly in women, can significantly influence Migraine Onset. Many women report experiencing migraines around their menstrual cycles, highlighting the connection between estrogen levels and headache frequency. A study published in Headache: The Journal of Head and Face Pain found that hormonal changes are among the most common triggers for women with migraines.
This hormonal link suggests that women should consider tracking their cycles alongside their migraine occurrences. Understanding the timing of these hormonal shifts can help in anticipating and managing migraines more effectively. Consultation with a healthcare provider may also reveal treatment options tailored to the individual's hormonal fluctuations.
The Importance of Lifestyle Factors
Aside from food, environmental influences, and hormonal changes, Lifestyle Factors play a crucial role in managing migraine triggers. Regular exercise, adequate hydration, and consistent sleep patterns can mitigate the frequency and severity of migraines. Engaging in physical activity can release endorphins, which may help buffer pain sensations. It's not just about what you eat.
Establishing a stable daily routine is essential. Chaos and unpredictability in sleep and meal schedules can contribute to the likelihood of migraines. By adopting a disciplined approach to daily life, including balanced meals and regular sleep hours, individuals may better navigate potential migraine triggers and minimize their impact.
For those who lead a busy lifestyle, integrating small changes can yield significant benefits. For example, incorporating short breaks during work can help alleviate tension and reduce stress-induced headaches, demonstrating how lifestyle adjustments can effectively contribute to migraine management.
Seeking Professional Help for Migraine Management
If the misconception that food is the sole migraine trigger persists in your life, it might be helpful to consult with a healthcare professional. They can provide tailored advice on identifying triggers, appropriate dietary modifications, and preventive medication options. A multidisciplinary approach often yields the best results for migraine sufferers, encompassing dietary advice, pain management strategies, and psychological support.
In conclusion, while diet plays a role, it is essential to consider the broader spectrum of migraine triggers. Your unique triggers may involve a combination of lifestyle factors, environmental influences, and hormonal changes. A comprehensive management plan that addresses all these facets can lead to better migraine control and an improved quality of life.
Myth 4: You Can Suffer Through a Migraine without Treatment
Understanding the Impact of Untreated Migraines
Many people believe that they can simply tough it out when it comes to migraine attacks, thinking that the symptoms will eventually subside. However, this misconception can lead to more severe and prolonged pain. Research shows that untreated migraines can last anywhere from hours to several days, and the pain can become debilitating. The longer you delay treatment, the more likely you are to experience increased intensity and frequency of attacks.
Moreover, Chronic Migraines can also result in additional health issues, including anxiety and depression. Studies have indicated that individuals suffering from chronic migraines are more likely to develop mood disorders, which in turn, can increase their pain levels. Addressing migraines early with proper treatment not only alleviates the pain but can also significantly improve overall mental health.
Effective Treatment Options for Migraines
When it comes to combating migraines, a variety of treatment options are available, ranging from over-the-counter medications to prescribed treatments. For instance, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can be effective for mild to moderate migraines. For more severe cases, doctors may prescribe triptans, which target specific migraine pathways in the brain to relieve symptoms quickly.
- Over-the-counter medications: Simple pain relievers and NSAIDs.
- Prescribed medications: Triptans and preventive treatments.
- Alternative therapies: Acupuncture and cognitive behavioral therapy.
Additionally, adopting lifestyle changes—like maintaining adequate hydration, regular sleep patterns, and a balanced diet—can serve as preventive measures. Engaging in stress-reduction techniques such as yoga or meditation can also decrease the frequency of migraines. Patients are encouraged to consult with healthcare professionals to create a personalized treatment plan that's tailored to their specific requirements.
Myth 5: Migraines Are Only a Women's Problem
Understanding the Demographics of Migraines
Migraines are often stereotyped as a condition mainly afflicting women, but research indicates the prevalence of migraines in men is significant as well. According to a study published in the journal Headache, approximately 6% of men experience migraines, which is a noteworthy figure. This misconception arises partly from the hormonal influences that affect women, such as menstruation and menopause. These biological factors can exacerbate migraines, leading to an increased reporting of these conditions among females. However, it is essential not to overlook the male population affected by this debilitating disorder.
An important aspect to consider is how societal expectations may influence the perceptions of migraines in men and women. Men, who may feel societal pressures to exhibit toughness or stoicism, might underreport their migraine occurrences. This leads to a gap in understanding the true demographic spread of migraines. A recent survey showed that many men avoid seeking treatment for headaches because they perceive it as a sign of weakness. Consequently, such barriers prevent a clear understanding of how many men experience migraines.
Gender Differences in Migraine Symptoms and Treatment
While it's true that women typically report higher instances of migraines, the symptoms and triggers can vary significantly between genders. Research suggests that men may experience more severe pain during migraine attacks and are more prone to chronic migraines. Studies indicate that men are often less likely to seek medical care, which can lead to untreated and prolonged episodes. Understanding these differences can be pivotal for healthcare providers when diagnosing and treating patients experiencing migraines.
Additionally, treatment strategies may need to be tailored differently based on gender. Women frequently use oral contraceptives to manage migraine symptoms due to hormonal fluctuations, while men may benefit more from lifestyle modifications such as stress management techniques and dietary changes. This indicates a significant opportunity for healthcare providers to incorporate personalized medicine approaches into treatment plans. By recognizing that migraines are not solely a women's issue, healthcare practitioners can ensure that both men and women receive comprehensive care tailored to their individual needs.
Myth 6: Migraines Go Away with Age
Understanding the Misconception
Migraines are often thought to be a condition that gradually fades away with aging. This belief is rooted in the observation that some individuals experience a diminishing frequency of attacks as they grow older. However, this is not universally true; many people continue to suffer from chronic migraines well into their later years. A study published in the journal Headache indicates that while some patients do report decreased migraine frequency, others may find that their symptoms persist or evolve into different forms.
It’s crucial to understand that migraine attacks can manifest differently at various stages of life, which might contribute to the misunderstanding of their frequency and severity. Hormonal changes, lifestyle shifts, and overall health status can impact how migraines are experienced as people age. Thus, assuming that migraines will simply go away with time can lead to inadequate management of the condition, increasing the burden of pain and disability.
Research Insights on Age and Migraines
Research provides significant insights into the relationship between age and migraine prevalence. A large-scale epidemiological study indicated that while some individuals report a decrease in migraine intensity with age, others develop new types or report worsened symptoms, especially post-menopause. The variability in experiences highlights the need for Individualized Treatment plans that can address the unique patterns of each patient.
Additionally, according to a report by the American Migraine Foundation, older adults may also be at risk for medication overuse headaches, particularly if they have relied on medication for long-term pain relief. Misconceptions surrounding age can lead to a lack of appropriate care or insufficient testing for underlying conditions that might contribute to persistent migraines.
Personal Strategies for Dealing with Migraines at Any Age
Regardless of age, effective management of migraines requires an individualized approach. Keeping a detailed migraine diary to track triggers, frequency, and reactions to medication can be invaluable. This record can help healthcare providers tailor treatment to meet specific patient needs. Moreover, lifestyle changes such as regular sleep patterns, hydration, and stress management techniques can also play a critical role in minimizing the frequency of attacks.
It’s equally important for individuals experiencing migraines, regardless of their age, to consult healthcare professionals for an accurate diagnosis and appropriate interventions. Emerging treatments, such as CGRP inhibitors and neuromodulation devices, have shown promise in providing relief and should be discussed with a healthcare provider. Staying informed about the latest research and treatment options can empower individuals to take charge of their health effectively.
Myth 7: Migraines Don’t Affect Your Life
Understanding the Impact of Migraines on Daily Activities
Migraines can severely disrupt daily life activities, including work, family responsibilities, and social engagements. Many individuals who suffer from migraines report that their ability to perform at work is significantly diminished, with studies indicating that 157 million workdays are lost annually due to this condition. For managers and coworkers, understanding the frequency and severity of a migraine can facilitate a more supportive and accommodating workplace. This awareness is crucial in creating an environment where individuals can manage their migraines while maintaining productivity.
Additionally, migraines can lead to missed social events and cherished moments. Many people find it challenging to make plans, fearing an episode will ruin the experience. This hesitation not only affects their social life but can also lead to feelings of isolation. Recognizing this, friends and family should be educated about the implications of migraines to foster empathy and support. Moreover, strategies like keeping a migraine diary or using apps for tracking triggers can provide insights and help individuals communicate their needs to their loved ones effectively.
Long-Term Consequences of Chronic Migraines
Chronic migraines can lead to long-term health issues, including increased anxiety and depression. Research shows that individuals with chronic migraines have a higher propensity to develop mental health disorders compared to the general population. This correlation may stem from the overwhelming pain and unpredictability of migraine attacks, which can severely impact one’s quality of life. It is essential for healthcare providers to screen for mental health conditions among migraine sufferers to ensure comprehensive care.
Additionally, the chronicity of migraines can hinder career advancement and personal development opportunities. Frequent absenteeism may result in strained relationships with colleagues and superiors, limiting growth potential and leading to job instability. Long-term migraine sufferers often find themselves caught in a cycle of underperformance and frustration. Therefore, implementing workplace accommodations and understanding the legal rights of those with chronic illnesses can mitigate some of these detrimental effects.
Addressing Misconceptions About Migraines
One prevalent misconception is that migraines are mere headaches, which can undermine the seriousness of the condition. Unlike regular headaches, migraines involve a complex interplay of neurological, genetic, and environmental factors. Recognizing the multifaceted nature of migraines is crucial in fostering appropriate understanding and treatment options. Education efforts aimed at dispelling these myths can significantly enhance societal attitudes towards migraine sufferers.
Moreover, individuals often believe that migraines are purely a personal struggle and do not impact the lives of those around them. In reality, family members, friends, and colleagues can be significantly affected. Modeling open conversations about migraines, triggers, and treatment options can promote a supportive atmosphere. Creating educational materials or hosting informational workshops can be effective ways to spread awareness and correct misconceptions.