Headache
Migraine Symptoms
HTML
Styling
CSS
Emergency
Health
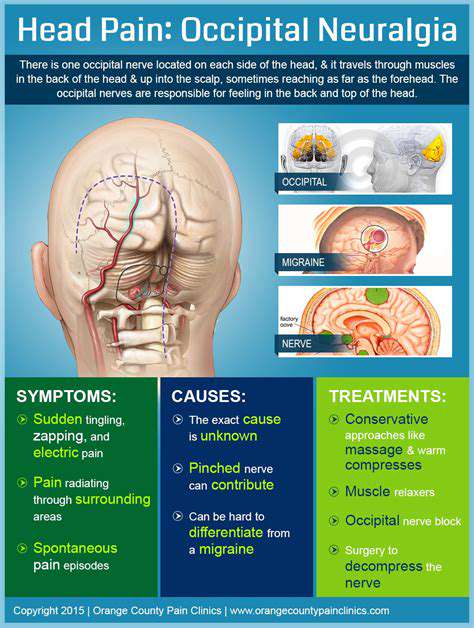
Types de maux de tête courants expliqués : De la tension aux céphalées en grappes
Les Douleurs Quotidiennes>
Migraines : Douleur pulsatile et symptômes associés
Comprendre la douleur migraineuse
La douleur migraineuse se manifeste généralement par une pulsation rythmique, habituellement concentrée d'un côté de la tête. Cette gêne atteint souvent des niveaux qui rendent les tâches quotidiennes
Quand consulter un médecin

Quand consulter immédiatement un médecin
Certains symptômes nécessitent une intervention médicale urgente, notamment l'apparition soudaine de douleurs musculaires sévères, une fièvre élevée, des difficultés respiratoires, des maux de tête intenses, des saignements importants ou une perte de conscience. Si vous présentez l'un de ces signes, veuillez contacter immédiatement les services d'urgence.
Read more about Types de maux de tête courants expliqués : De la tension aux céphalées en grappes
Comprendre la douleur pulsatile sur le côté gauche de la tête Explorez les complexités de la douleur pulsatile sur le côté gauche de la tête, avec des aperçus de ses symptômes, des causes courantes telles que les maux de tête de tension et les migraines, et des options de traitement efficaces. Ce guide complet examine les caractéristiques de la douleur pulsatile, y compris sa sensation de pulsation et sa nature intermittente, ainsi que les symptômes peut-être associés, comme les nausées et la sensibilité à la lumière. Découvrez comment les facteurs de style de vie, les déclencheurs environnementaux et les conditions médicales sous-jacentes peuvent contribuer à cet inconfort. Apprenez-en davantage sur les causes courantes telles que les migraines, les céphalées en grappes et l'artérite temporale, et comprenez quand il faut demander une attention médicale pour des symptômes graves. La page met également en lumière diverses stratégies de gestion, y compris des options de médication, des considérations diététiques et des modifications du mode de vie pour atténuer la douleur. Équipez-vous de connaissances pour gérer efficacement la douleur pulsatile et améliorer votre bien-être général.
Nov 09, 2024
L'Impact des Élongations Musculaires sur la Vie Quotidienne Explorez les effets significatifs des élongations musculaires sur le bien-être physique et mental. Cet article complet discute de la manière dont les élongations musculaires peuvent limiter les activités quotidiennes, réduire la force et l'endurance, et entraîner des douleurs chroniques si elles ne sont pas traitées. Découvrez les défis émotionnels et psychologiques associés aux blessures, y compris l'anxiété et les sentiments d'isolement. Découvrez des stratégies efficaces de prévention et de gestion, y compris des techniques d'échauffement appropriées et la méthode R.I.C.E. pour les soins immédiats. Comprenez les conséquences à long terme des élongations musculaires non traitées et l'importance de la réhabilitation pour une récupération complète. Équipez-vous de connaissances pour maintenir un mode de vie actif et sans blessures.
Nov 10, 2024
Causes et Remèdes
Ressentez-vous une douleur à l'avant gauche de votre tête ? Ce guide explore des causes courantes telles que le stress, les maux de tête de tension, les problèmes de sinus et les migraines. Découvrez des remèdes efficaces pour le soulagement, y compris des approches naturelles comme les huiles essentielles, l'hydratation et les techniques de relaxation. Apprenez quand consulter un professionnel de santé pour garantir des soins et une gestion appropriés des maux de tête persistants ou sévères. Restez informé et améliorez votre bien-être en comprenant et en abordant votre douleur à la tête.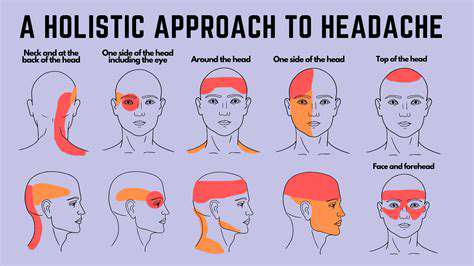 Points Clés : - Causes Courantes : Le stress, la tension, les problèmes de sinus et les migraines conduisent souvent à des douleurs à l'avant gauche de la tête. - Remèdes Efficaces : Utilisez des techniques de relaxation, restez hydraté et explorez des remèdes naturels pour le soulagement. - Conseils Médicaux : Sachez quand consulter un professionnel de santé pour des symptômes graves ou persistants. Renforcez-vous avec des connaissances et prenez des mesures proactives pour soulager la douleur à la tête !
Nov 19, 2024
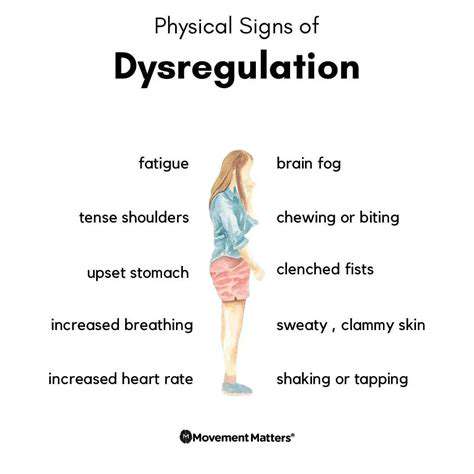
Comprendre les Symptômes Courants pour une Meilleure Gestion de la Santé. Explorez le guide essentiel pour reconnaître les symptômes physiques et mentaux courants qui peuvent indiquer des problèmes de santé sous-jacents. Cet article complet couvre l'importance d'identifier des symptômes tels que la fatigue, les changements d'appétit, la douleur et les troubles du sommeil, ainsi que des préoccupations en matière de santé mentale comme l'anxiété et la dépression. Apprenez quand demander une aide médicale et les mesures préventives que vous pouvez prendre pour maintenir votre bien-être. Renforcez-vous avec des connaissances pour améliorer votre santé et votre qualité de vie.
Dec 13, 2024
Comprendre la Tension Musculaire lors de la Toux : Causes, Symptômes et Stratégies d'ApaisementDescription Méta : Découvrez les causes de la tension musculaire due à la toux, les symptômes courants et des stratégies d'apaisement efficaces. Apprenez à prévenir et à gérer la tension musculaire pour améliorer votre santé respiratoire.---Quelles sont les causes de la tension musculaire lors de la toux ? La toux est un réflexe naturel destiné à dégager les voies respiratoires, mais elle peut entraîner des tensions musculaires, en particulier au niveau de la poitrine et de l'abdomen. Cet article explore les mécanismes derrière la tension musculaire lors de la toux, les facteurs aggravants courants et le rôle essentiel de la santé musculaire générale. Symptômes de la Tension Musculaire due à la Toux Apprenez à reconnaître des symptômes tels que douleur localisée, raideur et gonflement. Comprendre ces signes est crucial pour gérer l'inconfort et prévenir les problèmes chroniques. Mesures Préventives et Stratégies d'Apaisement Explorez des conseils pratiques pour prévenir les tensions musculaires causées par la toux, notamment en maintenant la santé respiratoire, l'hydratation et les techniques de respiration appropriées. Découvrez des méthodes d'apaisement efficaces, telles que la thérapie chaude et froide, les étirements doux et le moment où il est nécessaire de demander un avis médical. Renforcez votre santé Prenez des mesures proactives pour gérer votre santé en comprenant la relation entre la toux et la tension musculaire. Consultez des professionnels de la santé et engagez-vous dans des exercices pour renforcer vos muscles pour une meilleure résilience. Pour obtenir plus d'informations sur la prévention et la gestion des tensions musculaires lors de la toux, consultez notre guide complet !
Dec 31, 2024
La connexion entre la toux et la douleur à la têteExplorez la relation complexe entre la toux et la douleur à la tête dans notre guide complet. Découvrez comment les mécanismes physiologiques d'une toux peuvent entraîner des tensions musculaires, des maux de tête de tension et des migraines. Nous examinons des conditions courantes telles que la sinusite, la bronchite et les allergies qui aggravent les symptômes, ainsi que des problèmes sous-jacents potentiels nécessitant une attention médicale. Cette page offre des aperçus sur des techniques de gestion efficaces, des remèdes maison et des mesures préventives pour atténuer les symptômes et améliorer votre qualité de vie. Apprenez quand demander de l'aide si votre toux et vos maux de tête associés persistent ou s'aggravent. Comprenez mieux votre santé avec des connaissances qui vous permettent de communiquer efficacement avec les prestataires de soins de santé.
Dec 31, 2024
Symptômes, causes et remèdes
Ressentir une douleur à la partie inférieure gauche de la tête peut être préoccupant et perturbateur. Sur cette page, nous explorons les symptômes courants associés à cette affection, les causes possibles et les remèdes efficaces.
Apr 09, 2025
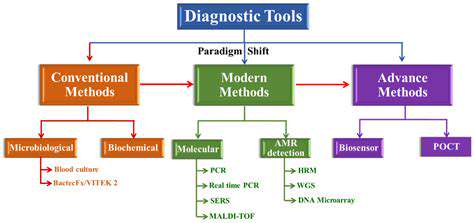
Diagnostiquer les migraines : Ce que votre médecin doit savoir
May 03, 2025
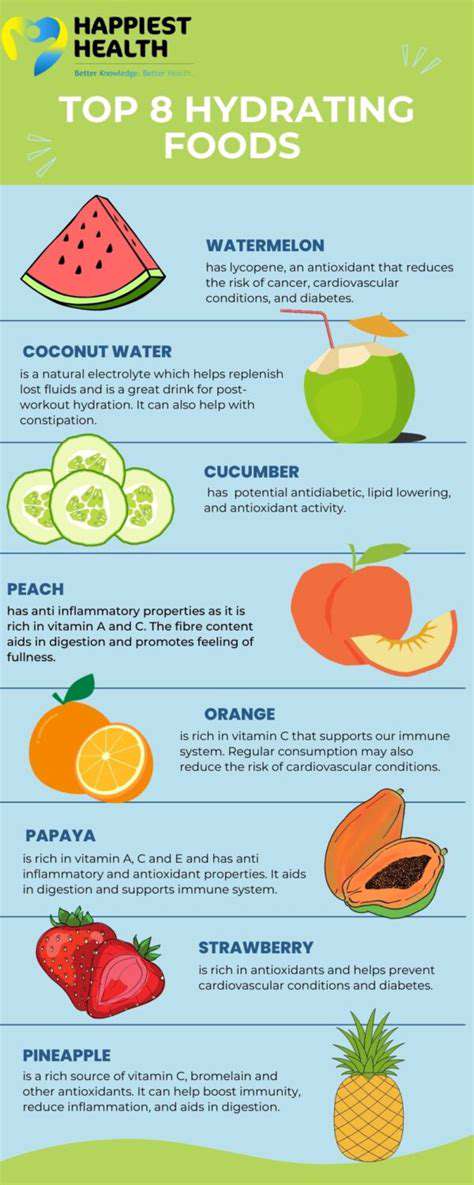
L'importance de l'hydratation pour la prévention des maux de tête
May 23, 2025
Gérer les migraines si vous avez un travail stressant
May 31, 2025
Comment soutenir un être cher souffrant de migraines
Jun 09, 2025
Comprendre les différentes formulations de médicaments contre la migraine (pilules, sprays nasaux, injections)
Jun 10, 2025