HTML
Styling
Headache
Pain Management
Neuroscience
Brain Function
CSS
Enxaquecas são apenas dores de cabeça fortes? Compreendendo a realidade
Desvendando a Complexidade das Migrenas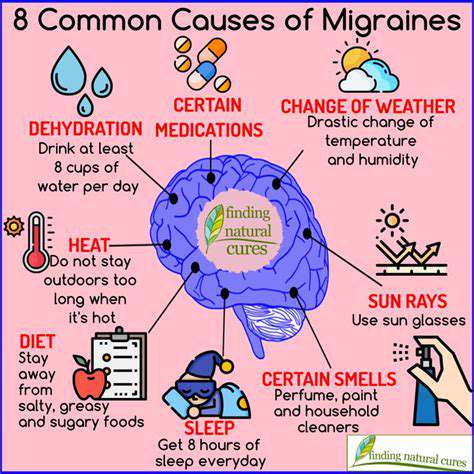
Características Distintivas da Dor de Enxaqueca
Compreendendo a Intensidade e a Pervasividade da Dor de Enxaqueca
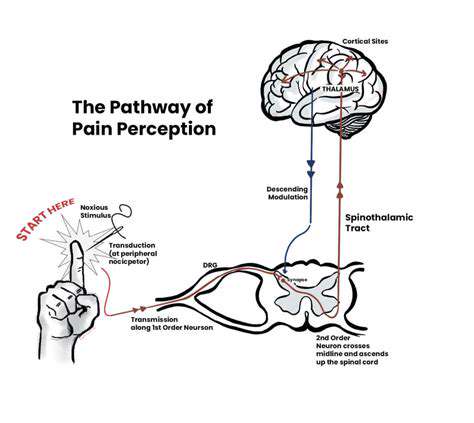
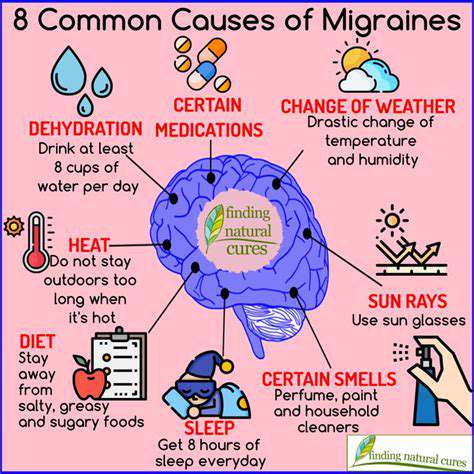
A dor de enxaqueca frequentemente transcende a experiência típica de uma dor de cabeça. É caracterizada por uma dor pulsátil
O Papel dos Fatores Neurológicos nas Migrenas
O Impacto da Estrutura Cerebral na Função
Read more about Enxaquecas são apenas dores de cabeça fortes? Compreendendo a realidade
Causas Comuns da Dor na Parte de Trás da Cabeça Explore as causas comuns da dor na parte de trás da cabeça, incluindo dores de cabeça tensionais, dores de cabeça cervicogênicas e enxaquecas. Conheça remédios e tratamentos eficazes, como medicamentos de venda livre, fisioterapia e terapias alternativas como acupuntura e quiropraxia. Entenda quando buscar atendimento médico e descubra medidas preventivas para reduzir a frequência e a gravidade das dores de cabeça. Este guia abrangente fornece informações sobre sintomas, estratégias de alívio e mudanças no estilo de vida para promover uma melhor saúde do pescoço e bem-estar geral.
Oct 14, 2024
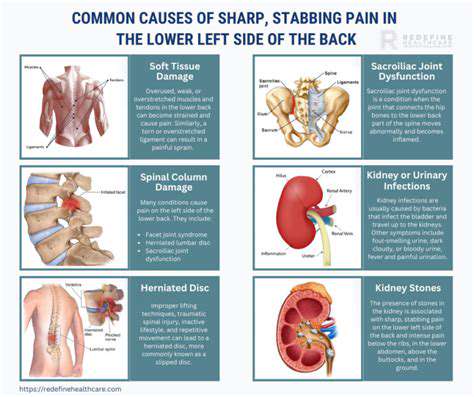
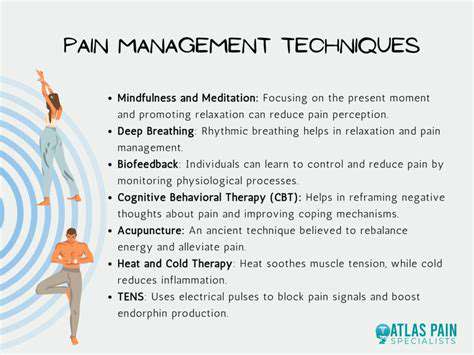
Entendendo a Dor Pulsante e Aguda Explore os aspectos críticos da dor pulsante e aguda neste guia abrangente. Descubra as características e causas comuns desses tipos de dor, incluindo enxaquecas, distúrbios vasculares, lesões e irritação nervosa. Aprenda a documentar seus sintomas de forma eficaz para um melhor diagnóstico e tratamento e entenda quando buscar atenção médica para episódios de dor urgentes. Esta página descreve várias opções de tratamento, desde medicamentos e terapias físicas até abordagens alternativas, e enfatiza a importância de estratégias de manejo personalizadas para melhorar a qualidade de vida. Ganhe insights valiosos sobre gatilhos de dor, práticas de autocuidado e a importância de consultas médicas oportunas para alívio ideal da dor.
Nov 19, 2024
Compreendendo a Dor de Cabeça, Pescoço e OmbrosExplore as causas multifacetadas da dor de cabeça, pescoço e ombros em nosso guia abrangente. Desde lesões musculares e tensão até enxaquecas e lesões na coluna, mergulhamos nos culpados comuns por trás do desconforto. Aprenda como fatores de estilo de vida, como postura e estresse, afetam significativamente os níveis de dor e descubra opções de tratamento eficazes, incluindo fisioterapia, medicamentos e abordagens holísticas como ioga e acupuntura. Nosso guia enfatiza a importância de medidas preventivas e quando procurar ajuda profissional para sintomas persistentes. Prepare-se com o conhecimento para gerenciar e aliviar a dor para uma melhor qualidade de vida.
Dec 28, 2024
A conexão entre tosse e dor de cabeçaExplore a relação intricada entre tosse e dor de cabeça em nosso guia abrangente. Descubra como a mecânica fisiológica de uma tosse pode levar a distensões musculares, dores de cabeça tensionais e enxaquecas. Investigamos condições comuns, como sinusite, bronquite e alergias, que agravam os sintomas, juntamente com possíveis problemas subjacentes que requerem atenção médica. Esta página oferece insights sobre técnicas de manejo eficazes, remédios caseiros e medidas preventivas para aliviar os sintomas e melhorar sua qualidade de vida. Aprenda quando procurar ajuda se a sua tosse e as dores de cabeça associadas persistirem ou piorarem. Entenda melhor a sua saúde com o conhecimento que lhe permite comunicar-se eficazmente com os profissionais de saúde.
Dec 31, 2024
Exercícios para os olhos para reduzir dores de cabeça relacionadas à fadiga ocular
May 13, 2025
Como as deficiências nutricionais podem contribuir para as dores de cabeça
May 23, 2025
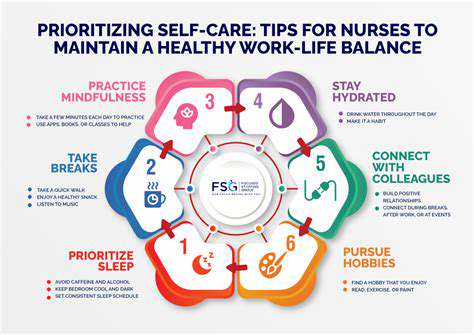
Gerenciando a Vida Social e Atividades com Migrañas
May 29, 2025
O uso de estimuladores de nervos periféricos para cefaleias
Jun 07, 2025
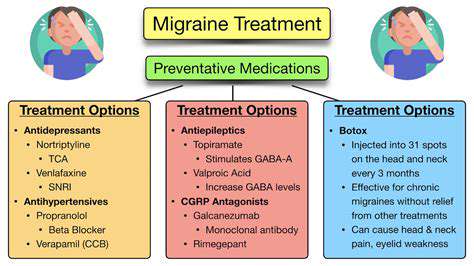
Medicamentos anticonvulsivantes usados para a prevenção da enxaqueca
Jun 24, 2025
A diferença entre enxaqueca episódica e crônica
Jul 08, 2025
Identificando seus padrões pessoais de gatilhos de enxaqueca
Jul 13, 2025