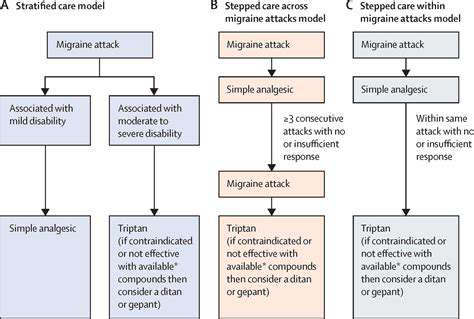
Migraine Management
Preventive Treatment
HTML
CSS
Thuốc điều trị chứng đau đầu nhức mỏi phòng ngừa: Khi nào cần dùng?
Xác định Thời Điểm Điều Trị Phòng Ngừa Phù Hợp
Hiểu về Nguyên Nhân Của Đau Đầu Buồn Nôn
Xác định những yếu tố cụ thể gây ra đau đầu là rất quan trọng để xác định thời điểm điều trị phòng ngừa tối ưu. Đau đầu...
Khả năng mắc các bệnh lý nền
Các bệnh lý nền tiềm ẩn góp phần gây đau nửa đầu
Xác định các bệnh lý nền tiềm ẩn là rất quan trọng để phát triển các chiến lược phòng ngừa đau nửa đầu hiệu quả. Mặc dù nhiều cơn đau nửa đầu là nguyên phát, có nghĩa là không xác định được nguyên nhân cụ thể, nhưng một số bệnh lý
Read more about Thuốc điều trị chứng đau đầu nhức mỏi phòng ngừa: Khi nào cần dùng?
Đau đầu bên trái khi cúi xuống: Hiểu về các triệu chứng
May 01, 2025
Đau đầu ở trẻ em: Khi nào cần lo lắng và những cách giúp đỡ nào?
May 07, 2025
Cân bằng giữa các phương pháp điều trị tự nhiên và phương pháp điều trị truyền thống
May 17, 2025
Chiến lược đối phó với cơn đau nửa đầu không thể dự đoán
May 25, 2025
Lợi ích tâm lý của việc theo dõi cải thiện chứng đau nửa đầu
May 26, 2025
Những bước nhỏ, tác động lớn: Cải thiện phúc lợi mỗi ngày
May 26, 2025
Đau đầu丛 và nguy cơ đột quỵ: Hiểu về mối liên hệ
May 27, 2025
Các Phương Pháp Điều Trị Tự Nhiên: Tăng Cường Khả Năng Chữa Lành Của Cơ Thể
May 31, 2025
Hiểu về Đau đầu cục bộ không đau: Các triệu chứng không đau
Jul 09, 2025
Kiểm soát Đau Đầu Bị Cơn: Các bước chủ động để quản lý
Jul 13, 2025
Thiết bị điều chỉnh thần kinh cho điều trị chứng đau đầu dữ dội (ví dụ: Cefaly, Nerivio)
Jul 14, 2025
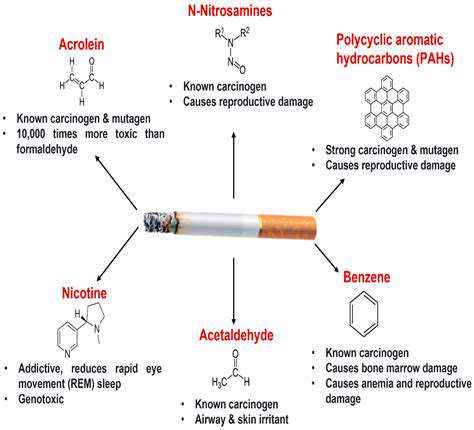
Tác động của hút thuốc lá và thuốc lá điện tử đến tần suất đau đầu
Jul 14, 2025