HTML
CSS
Pain Management
Preventive Care
Hiểu về Viêm Thần Kinh Bướm: Một Nguyên Nhân Gây Đau Đầu
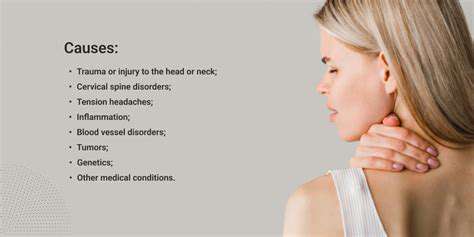
Nguyên nhân của đau thần kinh chẩm
Kích thích thần kinh chẩm
Một trong những nguyên nhân phổ biến nhất của đau thần kinh chẩm là kích thích các dây thần kinh chẩm. Những dây thần kinh này, bắt nguồn từ phần trên của
Quản lý và ngăn ngừa các đợt tái phát trong tương lai
Chiến lược quản lý chủ động
Quản lý chủ động đau thần kinh chẩm bao gồm một cách tiếp cận đa phương diện nhằm giảm thiểu nguy cơ tái phát trong tương lai và cải thiện sức khỏe tổng thể.
Read more about Hiểu về Viêm Thần Kinh Bướm: Một Nguyên Nhân Gây Đau Đầu
Khám phá hướng dẫn toàn diện về thuốc giảm đau, tập trung vào các loại khác nhau có sẵn cho quản lý đau mạn tính, bao gồm các tùy chọn không kê đơn và theo toa. Tìm hiểu về thuốc chống viêm không steroid (NSAIDs), opioids và các loại thuốc hỗ trợ như thuốc chống trầm cảm và thuốc chống co giật. Khám phá sự khác biệt giữa thuốc giảm đau tại chỗ và các biện pháp tự nhiên như liệu pháp hương liệu và trị liệu bằng mát xa, đồng thời hiểu rõ những rủi ro và lợi ích liên quan đến mỗi lựa chọn điều trị. Tham gia vào chiến lược quản lý đau cá nhân hóa kết hợp thay đổi lối sống và các liệu pháp mới nổi để có kết quả tối ưu. Tư vấn với các nhà cung cấp dịch vụ chăm sóc sức khỏe để tìm ra giải pháp giảm đau tốt nhất phù hợp với nhu cầu của bạn.
Oct 15, 2024
Hướng Dẫn Toàn Diện để Hiểu Biết về Đau Đầu và CổKhám phá các nguyên nhân phổ biến gây đau đầu và cổ, bao gồm căng cơ, đau đầu do căng thẳng và chấn thương. Tìm hiểu các chiến lược thực tế để quản lý cơn đau thông qua các bài tập trị liệu, thuốc và liệu pháp thay thế. Khám phá các thay đổi lối sống có thể ngăn ngừa các cơn đau và hiểu khi nào nên tìm kiếm sự giúp đỡ chuyên nghiệp cho các tình trạng mạn tính. Dù là cải thiện tư thế, sử dụng các kỹ thuật thư giãn, hay xem xét các phương pháp điều trị y tế, hướng dẫn này cung cấp những hiểu biết cần thiết để giúp bạn quản lý và giảm nhẹ đau đầu và cổ một cách hiệu quả.
Nov 02, 2024
Hiểu Đau Cổ Bên Trái: Nguyên Nhân, Triệu Chứng và Điều TrịKhám phá hướng dẫn toàn diện về đau cổ bên trái, bao gồm nguyên nhân, triệu chứng và các lựa chọn điều trị hiệu quả. Tìm hiểu cách các yếu tố như căng cơ, tư thế kém và các tình trạng y tế tiềm ẩn góp phần vào sự khó chịu, và tìm hiểu về tầm quan trọng của chẩn đoán chính xác và can thiệp sớm. Bài viết của chúng tôi cũng làm nổi bật các chiến lược điều trị thực tế, bao gồm vật lý trị liệu, chăm sóc chỉnh hình và điều chỉnh lối sống để ngăn ngừa tái phát. Dù bạn đang tìm kiếm sự giảm nhẹ hay muốn hiểu rõ hơn về cơn đau của mình, tài nguyên này cung cấp những hiểu biết quý giá để giúp bạn quản lý hiệu quả chứng đau cổ bên trái.
Nov 25, 2024
Khám phá nguyên nhân, triệu chứng và tùy chọn điều trị cho đau ở bên trái đầu và tai. Hướng dẫn toàn diện này đi sâu vào các điều kiện phổ biến như đau đầu căng thẳng, đau nửa đầu, nhiễm trùng tai và rối loạn khớp thái dương hàm (TMJ). Học cách xác định các triệu chứng đi kèm, hiểu khi nào cần tìm kiếm sự chăm sóc y tế và khám phá các biện pháp khắc phục tại nhà cũng như các phương pháp điều trị không kê đơn hiệu quả. Giữ thông tin về các tình trạng nghiêm trọng có thể cần chăm sóc khẩn cấp và tìm hiểu về các biện pháp phòng ngừa để quản lý đau đầu và khó chịu ở tai. Cải thiện chất lượng cuộc sống của bạn với những lời khuyên thực tiễn và các khuyến nghị của chuyên gia để làm giảm cơn đau ở bên trái đầu và tai.
Dec 04, 2024
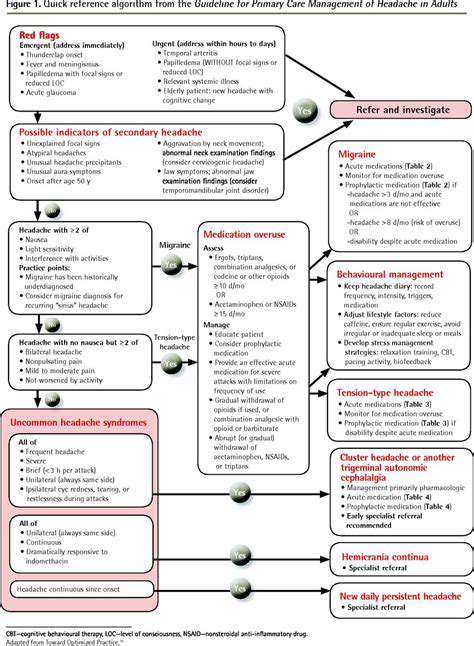
Vai trò của bác sĩ chăm sóc sức khỏe ban đầu trong quản lý đau đầu
May 03, 2025
So sánh các loại nhật ký và công cụ theo dõi đau đầu khác nhau
May 12, 2025
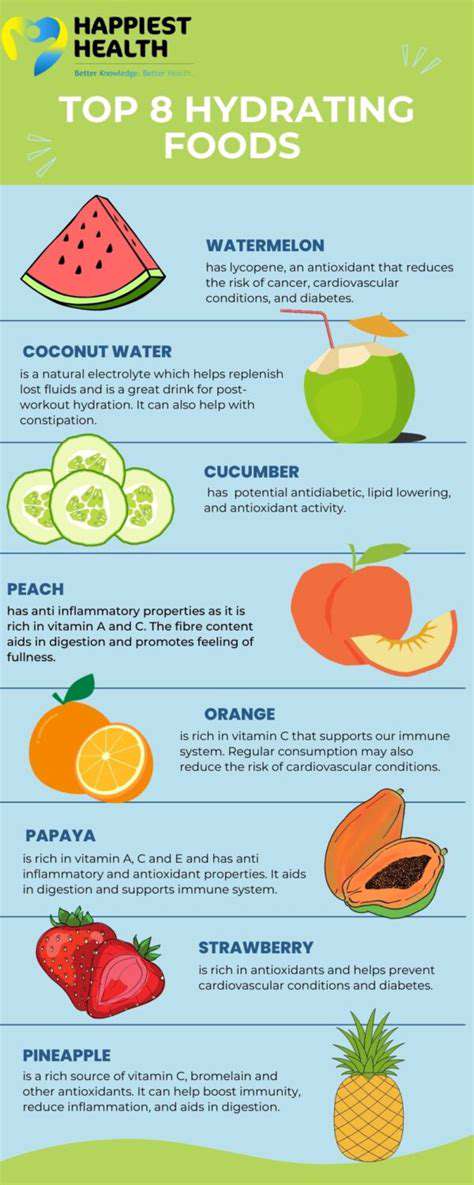
Vai trò của việc giữ nước trong việc ngăn ngừa đau đầu
May 23, 2025
Hiểu về đau đầu do cổ: Khi đau cổ gây ra đau đầu
Jun 04, 2025
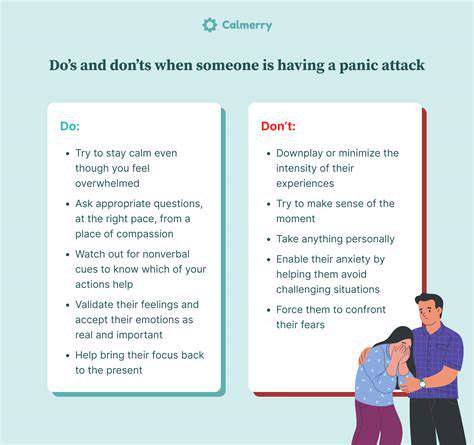
Làm thế nào để hỗ trợ người thân yêu bị đau nửa đầu?
Jun 09, 2025
Nguyên nhân thực sự của chứng đau nửa đầu là gì? Khám phá khoa học
Jun 10, 2025
Đau đầu叢 trong phụ nữ: Ảnh hưởng của hormone suốt cuộc đời
Jul 14, 2025
Xây dựng kế hoạch ứng phó khẩn cấp cho tình trạng đau nửa đầu kéo dài
Jul 18, 2025