Cognitive Behavioral Therapy (CBT) for Chronic Pain Management
- Assuming the worst possible outcome will occur
- Viewing temporary setbacks as permanent failures
- Focusing exclusively on negative aspects while ignoring positive developments
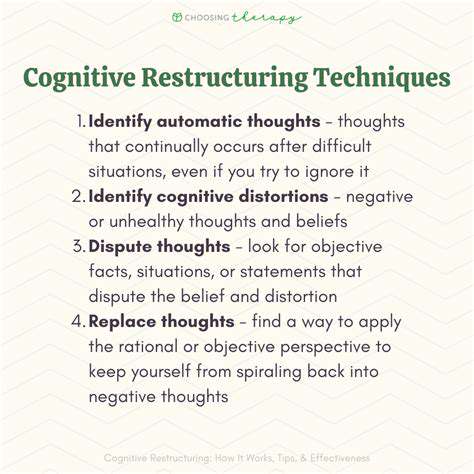
Therapeutic techniques provide practical tools to evaluate these thoughts critically. Patients learn to ask themselves important questions: What evidence supports this thought? Is there another way to look at this situation? How would I advise a friend in this position? This process of examination often reveals that our initial interpretations are more extreme than the reality warrants.
Developing Practical Coping Strategies
Beyond changing thought patterns, this approach provides concrete methods for managing difficult moments. Relaxation practices help calm both mind and body, creating physiological changes that can reduce discomfort. Simple breathing techniques, when practiced regularly, can become powerful tools for interrupting the stress-pain cycle.
Stress management plays a crucial role, as tension often exacerbates physical symptoms. Learning to recognize early signs of stress and having prepared responses can prevent minor discomfort from escalating into major episodes. Many patients find that keeping a toolbox of quick stress-relief methods gives them greater confidence in handling challenging situations.
Behavioral Activation and Activity Level
It's natural to want to avoid activities when experiencing discomfort, but this often backfires over time. Therapeutic approaches encourage gradual re-engagement with meaningful activities through careful pacing. The key lies in finding the right balance - enough activity to maintain function and enjoyment, but not so much as to cause excessive strain.
This process often involves:
- Breaking tasks into smaller, manageable steps
- Alternating activity with rest periods
- Tracking progress to identify patterns and make adjustments
Over time, this methodical approach helps rebuild confidence and demonstrates that activity doesn't necessarily lead to increased suffering. Many patients discover they're capable of more than they initially believed possible.
Mindfulness and Acceptance Techniques
Rather than fighting against discomfort, mindfulness teaches a different approach - observing sensations without judgment or resistance. This doesn't mean giving up or resigning oneself to suffering. Instead, it's about changing our relationship to the experience. When we stop struggling against what we can't change, we often find we have more energy available for what we can influence.
Simple mindfulness exercises might involve focusing on the breath while acknowledging sensations without trying to alter them. This practice can create mental space between the person and their experience, reducing the sense of being overwhelmed or controlled by symptoms.
Setting Realistic Goals and Expectations
Effective management requires honest assessment and flexible goal-setting. Complete elimination of symptoms may not be realistic, but meaningful improvement in quality of life absolutely is. The therapeutic process helps individuals identify what better looks like for them personally - whether that's being able to play with grandchildren, return to work, or simply sleep through the night.
Goals should be:
- Specific and measurable
- Attainable yet challenging
- Time-bound with clear milestones
- Regularly reviewed and adjusted as needed
This structured approach provides a roadmap for progress while allowing for the inevitable ups and downs of the healing process. Celebrating small victories along the way helps maintain motivation and reinforces positive changes.
Behavioral Techniques for Managing Pain and Activities
Cognitive Restructuring
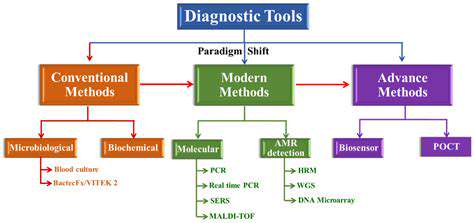
Thought reframing stands as a fundamental component of comprehensive pain management strategies. Automatic negative thoughts often arise without conscious intention, yet they powerfully shape our experience. Common problematic patterns include:
- Catastrophic predictions (This will never get better)
- Overgeneralization (Because I hurt today, I'll always hurt)
- Mental filtering (Focusing only on negative aspects while ignoring positives)
The restructuring process involves several steps:
- Identifying the automatic thought
- Examining the evidence for and against it
- Generating alternative interpretations
- Testing these alternatives through behavioral experiments
For instance, someone who thinks I can't do anything productive when I'm in pain might keep a log of activities actually accomplished despite discomfort. The accumulated evidence often contradicts the initial pessimistic belief, creating space for more balanced thinking.
Relaxation Techniques
Physical tension frequently accompanies and amplifies discomfort, creating a vicious cycle. Various relaxation methods can interrupt this pattern:
Progressive muscle relaxation teaches awareness of tension and the ability to release it systematically. Moving through muscle groups from feet to head, individuals learn to recognize subtle tension they may have been carrying unconsciously.
Controlled breathing exercises activate the body's natural relaxation response. A simple technique involves inhaling for a count of four, holding briefly, then exhaling for a count of six. This slightly prolonged exhalation triggers physiological calming.
Guided imagery uses the power of imagination to create sensory-rich mental experiences that promote relaxation. Visualization of peaceful settings - perhaps a quiet beach or mountain stream - can provide temporary respite from discomfort while reducing overall stress levels.
Behavioral Activation
When pain persists, people naturally begin avoiding activities they associate with increased discomfort. Unfortunately, this avoidance often leads to:
- Reduced physical conditioning
- Social isolation
- Loss of enjoyable experiences
- Increased focus on symptoms
Behavioral activation systematically reverses this pattern through gradual exposure to avoided activities. The process typically involves:
- Identifying valued activities that have been reduced or eliminated
- Breaking them into manageable steps
- Scheduling them at manageable intensity
- Monitoring both enjoyment and discomfort levels
This method helps disprove the fear that activity automatically leads to unbearable pain. Many patients are surprised to discover they can still derive satisfaction from adapted versions of previously enjoyed pursuits.
Pain Coping Strategies
Developing a personalized toolkit of coping methods empowers individuals to handle flare-ups more effectively. Useful strategies might include:
- Pacing activities with regular breaks
- Using heat/cold therapy as appropriate
- Practicing brief mindfulness exercises during difficult moments
- Engaging in pleasant distractions
Social support plays a crucial role in effective coping. Connecting with others who understand the challenges of chronic pain can reduce feelings of isolation. Support groups provide opportunities to share practical tips while receiving emotional validation. Even a single understanding friend or family member can make a significant difference in maintaining motivation during difficult periods.
Lifestyle Changes and Long-Term Management

Prioritizing Physical Activity
Movement matters profoundly for managing persistent discomfort. While intense exercise may not be appropriate, regular gentle activity provides multiple benefits:
- Maintains joint mobility and muscle strength
- Releases natural pain-relieving endorphins
- Improves sleep quality
- Boosts mood and reduces stress
The key lies in finding the right type and amount of movement for each individual's unique situation. Water-based activities often work well as they reduce impact while providing resistance. Simple walking programs, starting with very short distances and gradually increasing, can be surprisingly effective. The most important factor is consistency rather than intensity.
Adopting a Balanced Diet
Nutrition plays a subtle but significant role in pain management. While no specific pain diet exists, certain dietary approaches may help:
- Anti-inflammatory foods (fatty fish, leafy greens, berries)
- Adequate hydration
- Balanced blood sugar through regular meals/snacks
- Reducing processed foods and excess sugar
Some individuals find that certain foods seem to trigger or worsen their symptoms. Keeping a food-symptom diary can help identify potential connections. Small, sustainable changes often prove more effective than drastic dietary overhauls that are difficult to maintain.
Managing Stress Effectively
Since stress reliably exacerbates pain perception, developing robust stress-management skills is essential. Different approaches work for different people:
- Mindfulness meditation (even 5-10 minutes daily)
- Gentle yoga or tai chi
- Creative expression (art, music, writing)
- Nature exposure (park walks, gardening)
Identifying personal stress triggers allows for proactive management. For unavoidable stressors, having prepared coping strategies makes them more manageable. Regular practice of stress-reduction techniques builds resilience over time, making them more effective when truly needed.
Prioritizing Sleep and Rest
The relationship between sleep and pain is bidirectional - pain disrupts sleep, while poor sleep lowers pain thresholds. Improving sleep hygiene can significantly impact daytime functioning:
- Consistent bedtime/waking schedule
- Cool, dark, quiet sleep environment
- Screen-free wind-down routine
- Comfortable sleep positioning
For those whose pain frequently interrupts sleep, strategic napping (limited to 20-30 minutes) can help compensate without disrupting nighttime sleep patterns. Quality rest should be viewed as an essential component of pain management, not a luxury. Small improvements in sleep often lead to noticeable reductions in daytime symptom intensity.