Comparing Different Types of Preventive Migraine Medications
Mechanism of Action
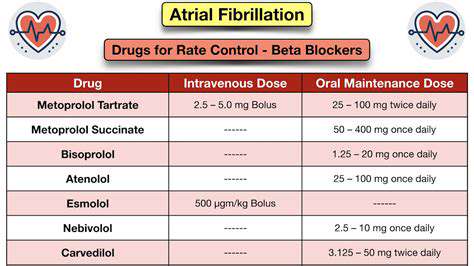
Beta-blockers, a class of medications, exert their therapeutic effects by blocking the action of adrenaline and noradrenaline, also known as epinephrine and norepinephrine. These neurotransmitters play a crucial role in the body's response to stress and stimulation, influencing heart rate, blood pressure, and other physiological functions. By inhibiting their binding to beta-adrenergic receptors, beta-blockers effectively dampen the sympathetic nervous system's influence, leading to a reduction in heart rate and blood pressure. This mechanism is fundamental to their use in treating a wide range of cardiovascular conditions.
The precise way in which beta-blockers achieve these effects can vary slightly depending on the specific type of beta-blocker. For example, some beta-blockers are more selective for beta-1 receptors, found primarily in the heart, resulting in a more pronounced effect on cardiac function. Others have a broader effect, impacting both beta-1 and beta-2 receptors. Understanding these nuances helps clinicians tailor treatment strategies to individual patient needs.
Clinical Applications
Beta-blockers are widely used to treat a variety of conditions, primarily those related to the cardiovascular system. A significant application is in the management of hypertension, where their ability to lower blood pressure makes them a cornerstone of treatment. They also play a vital role in reducing the risk of heart attack and stroke, particularly in individuals with a history of these events.
Beta-blockers are often prescribed to patients with angina, a condition characterized by chest pain due to reduced blood flow to the heart. By decreasing the workload on the heart, beta-blockers can help alleviate angina symptoms. Furthermore, they are frequently used in the treatment of arrhythmias, abnormal heart rhythms, helping to regulate the heart's electrical activity and restore a normal rhythm. They are also used in the treatment of some specific types of migraine headaches.
Their use extends beyond the cardiovascular system in certain cases. Beta-blockers can be helpful in managing anxiety and tremor, though these applications are often secondary to their primary use in cardiovascular conditions.
It's important to remember that the specific type of beta-blocker and the dosage prescribed will depend on the individual patient's condition and needs. A doctor will carefully consider these factors when determining the most appropriate treatment plan.
The long-term use and efficacy of beta-blockers require careful monitoring of the patient's response. Regular check-ups and blood pressure measurements are essential to ensure that the treatment is effective and safe.
Modern maintenance strategies now prioritize anticipating equipment failures before they happen. This forward-thinking method enables companies to plan repairs during scheduled downtimes, avoiding expensive and disruptive emergency fixes. The outcome is a dramatic decrease in unplanned outages, reducing production losses while extending machinery lifespan. When businesses implement these predictive approaches, they often achieve more stable operational outputs without the constant worry of sudden breakdowns.
Anti-CGRP Medications: A Novel Approach to Migraine Prevention
Understanding CGRP and Its Role in Migraine
CGRP, or calcitonin gene-related peptide, is a neuropeptide that plays a significant role in the transmission of pain signals in the nervous system. While its precise function is still being investigated, research strongly suggests that CGRP's influence on the nervous system contributes to the inflammatory and vasodilation processes that are believed to be crucial components of migraine attacks. This understanding of CGRP's involvement has led to the development of innovative therapies focusing on blocking its activity.
Numerous studies have highlighted the elevated levels of CGRP in the cerebrospinal fluid during migraine attacks. This correlation underscores the potential of targeting CGRP as a primary method for preventing and managing migraine episodes. This approach distinguishes itself from traditional migraine treatments, which often focus on symptom relief rather than addressing the underlying mechanisms.
Mechanism of Action of Anti-CGRP Medications
Anti-CGRP medications work by either neutralizing CGRP or blocking its receptors. This disruption of CGRP's activity effectively reduces the inflammatory response and the vasodilation that are thought to trigger migraine pain. These medications, delivered through various routes such as injections or nasal sprays, achieve this by binding to CGRP molecules or their receptors, preventing them from activating pain pathways in the brain.
The specific mechanisms of action may differ slightly between various anti-CGRP drugs. However, the common thread is the inhibition of CGRP's influence on the nervous system, thereby limiting the cascade of events that leads to a migraine attack. This targeted approach is a significant advancement in migraine management compared to older therapies that often address symptoms rather than the root cause.
Types of Anti-CGRP Medications and Their Delivery Methods
Different anti-CGRP medications are available, each employing slightly distinct approaches for inhibiting CGRP activity. Some medications work by binding to CGRP directly, neutralizing its effect, while others target the receptors that CGRP interacts with, preventing the activation of pain pathways. These medications offer varied delivery methods, including injections, nasal sprays, and oral options. The choice of administration method often depends on individual patient preferences and healthcare provider recommendations.
Efficacy and Safety Profile of Anti-CGRP Medications
Extensive clinical trials have demonstrated the significant efficacy of anti-CGRP medications in reducing the frequency and intensity of migraine attacks. Studies have consistently shown that these medications can effectively decrease the number of migraine days experienced by patients, leading to improvements in overall quality of life. However, like any medication, anti-CGRP therapies have potential side effects, although these are generally mild and transient.
Safety data from various clinical trials suggests that the side effects of anti-CGRP medications are generally manageable. Common side effects may include injection site reactions, nasal congestion (with nasal sprays), or mild gastrointestinal discomfort. Healthcare professionals carefully monitor patients for any adverse reactions to ensure the benefits outweigh potential risks.
Comparing Anti-CGRP Medications to Other Migraine Prevention Strategies
Anti-CGRP medications represent a novel approach to migraine prevention, offering a targeted strategy that addresses the underlying mechanisms of the condition. When compared to other preventive therapies, such as beta-blockers or tricyclic antidepressants, anti-CGRP medications often demonstrate superior efficacy in reducing migraine frequency and intensity. This makes them a strong consideration for patients seeking comprehensive migraine management strategies.
While other preventive strategies exist, anti-CGRP medications stand out due to their specific targeting of CGRP. This targeted approach often results in greater effectiveness and fewer side effects compared to some other preventive methods. This makes anti-CGRP medications a valuable addition to the range of options available for migraine sufferers.