Debilitating Stabbing Head Pains Relief and Prevention Strategies for Chronic Migraine Sufferers
Migraine Causes and Triggers
Understanding the Physiological Causes of Migraines
The mechanisms behind migraines remain relatively complex, involving several biological factors. A major contributing factor is the dysfunction in the brain's pathways, which may lead to changes in blood flow and inflammation. Studies indicate that genetic predispositions can also play a significant role, underscoring how migraines can sometimes run in families.
Furthermore, neurochemical imbalances, particularly involving serotonin, dopamine, and other neurotransmitters, can trigger migraine attacks. These imbalances often lead to heightened sensitivity in the nervous system, resulting in intense pain. This biological complexity makes understanding individual triggers crucial for managing and alleviating symptoms.
Common Environmental Triggers of Migraines
Environmental factors have been shown to exacerbate migraine conditions significantly. Common triggers include bright lights, strong odors, and significant temperature changes. People living in urban areas may find that air pollution also contributes to the frequency and severity of their attacks.
Additionally, changes in weather, such as barometric pressure fluctuations, can also serve as a trigger. Individuals suffering from chronic migraines should keep a diary to pinpoint how environmental elements correlate with their symptoms, aiding in prevention strategies.
Dietary Influences on Migraine Occurrence
The food we consume can deeply impact migraine frequency and intensity. Certain foods, such as aged cheeses, processed meats, and foods containing MSG, are known triggers for many migraine sufferers. Keeping a detailed food journal can help individuals identify which dietary components lead to their migraines.
Moreover, dehydration is another significant factor that can predispose someone to an attack. Ensuring regular fluid intake, along with maintaining a balanced diet rich in nutrients, can help mitigate migraine occurrences. By making mindful choices regarding diet, chronic sufferers can work towards reducing the number and severity of their attacks.
Emotional and Psychological Triggers of Migraines
Migraine sufferers often report emotional stress as a prominent trigger for their pain. Conditions such as anxiety and depression can amplify migraine occurrences, creating a vicious cycle of pain and emotional distress. Stress management techniques, such as meditation and yoga, can be beneficial in reducing overall stress levels and, subsequently, the frequency of migraines.
Moreover, lack of sleep or irregular sleep patterns can also lead to increased migraine attacks. Establishing a consistent sleep schedule is crucial since both oversleeping and sleep deprivation can aggravate migraines. Understanding the relationship between emotional health and migraines can empower individuals to seek effective coping mechanisms.
Diagnosis and Treatment Options
Understanding the Diagnosis of Chronic Migraines
Diagnosing chronic migraines involves a comprehensive assessment of a patient's medical history and symptoms. Medical professionals often take into account the frequency, intensity, and type of pain experienced by the patient. This thorough understanding is essential to differentiate chronic migraines from other types of headaches, which can significantly impact treatment decisions.
A detailed symptom diary can be an invaluable tool in the diagnostic process. Patients are encouraged to log when headaches occur, their duration, associated symptoms, and any potential triggers. This documentation helps healthcare providers identify patterns and contribute to a more accurate diagnosis.
Healthcare providers may also perform neurological examinations to assess any possible underlying conditions. These examinations typically include checking vision, coordination, and sensory response. Any unusual findings may lead to further imaging tests, such as MRI or CT scans, to rule out other serious conditions potentially mimicking migraines.
Another key aspect of diagnosing migraines includes exploring a patient's family history of headaches or migraines. A hereditary factor can greatly influence the frequency and severity of migraines. Gathering this information offers crucial insights and assists in formulating a tailored treatment plan.
Finally, patient education plays a fundamental role in the diagnosis of chronic migraines. Empowering patients with knowledge about their condition facilitates open communication with healthcare providers and encourages proactive management of symptoms, ensuring a more effective approach to treatment.
Treatment Options for Chronic Migraines
When it comes to treating chronic migraines, there is no one-size-fits-all solution. Treatments vary widely based on the severity, frequency, and individual triggers of migraines. Acute medications, such as triptans, are often prescribed to help alleviate symptoms during migraine attacks, providing significant relief for many patients with timely usage.
Preventative treatments are equally important for chronic migraine sufferers. Daily medications such as beta-blockers, anticonvulsants, and certain antidepressants can significantly reduce the frequency and intensity of migraine attacks. Finding the right combination may require patience and consultation with healthcare professionals.
In recent years, new treatment modalities have emerged, including botulinum toxin injections and CGRP (calcitonin gene-related peptide) inhibitors. These innovative treatments have shown promise for patients who do not respond adequately to traditional medications, offering a new lease on life for many migraine sufferers.
Additionally, lifestyle modifications can enhance treatment efficacy. Patients are encouraged to identify and avoid specific triggers, such as certain foods, stress, and sleep disturbances. Incorporating relaxation techniques, regular exercise, and a balanced diet can not only help reduce the frequency of migraines but also improve overall well-being.
Ultimately, treatment for chronic migraines requires a multi-faceted approach where ongoing evaluation and adjustment of strategies are crucial. Regular follow-up consultations with healthcare providers can help to fine-tune treatment plans, ensuring that patients find the best possible balance between managing their migraines effectively and maintaining a high quality of life.
Emerging Research and Future Directions
Research into chronic migraines is continuously evolving, paving the way for more effective treatments tailored to individual needs. One exciting area of investigation focuses on the biological mechanisms that trigger migraines. Understanding these pathways may lead to the development of targeted therapies that address the root causes rather than merely alleviating symptoms.
Clinical trials exploring novel medications and treatment techniques are underway, showing potential benefits for migraine sufferers. Therapies using neuromodulation techniques, such as transcranial magnetic stimulation (TMS), have shown preliminary success, potentially providing patients with a non-invasive option for quick relief from migraine attacks.
Another significant area of research is the role of diet and nutrition in managing migraines. Recent studies suggest that certain dietary supplements may reduce the frequency of migraine attacks. As more data comes to light, personalized dietary recommendations could become an integral part of migraine management strategies.
Furthermore, advancements in technology are contributing to better management of chronic migraines. Wearable devices that track symptoms and triggers can provide valuable insights into headache patterns, thereby assisting both patients and doctors in making informed treatment decisions. This integration of technology in healthcare fosters a more proactive approach to managing migraines.
As our understanding of chronic migraines deepens, collaboration among researchers, healthcare providers, and patients remains vital. Collective efforts are essential to unravel the complexities of migraines, ultimately leading to more effective prevention and treatment strategies that enhance the quality of life for chronic migraine sufferers.
Stabbing Head Pains Relief and Prevention Strategies
Understanding Stabbing Head Pains
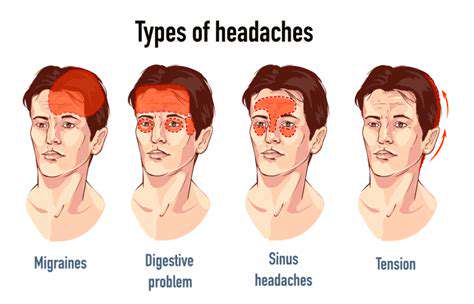
Stabbing head pains, often referred to as migraines, manifest as intense, pulsing pain on one side of the head. This debilitating condition may occur sporadically or frequently, severely impacting daily activities and quality of life. Understanding the unique nature of these headaches is crucial for effective management. Individuals often describe the pain as sharp and piercing, creating a sense of urgency for relief.
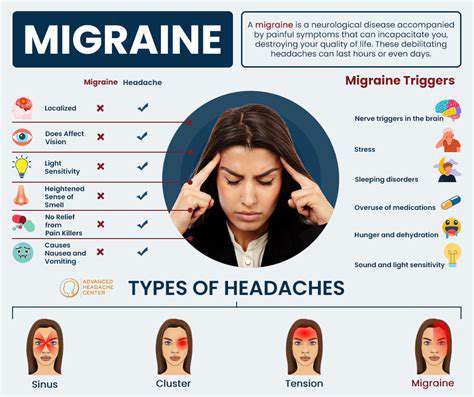
Migraine sufferers may experience accompanying symptoms such as nausea, sensitivity to light, and heightened sound sensitivity, complicating their condition. It is essential to recognize that not all headaches are migraines; they exist within a spectrum that includes tension headaches and cluster headaches. By identifying the characteristics of stabbing pains, individuals can better articulate their experiences to healthcare professionals.
Triggers for these stabbing head pains can vary significantly among individuals. Common factors include hormonal changes, stress, certain foods, and even changes in weather. Keeping a migraine diary can help pinpoint specific triggers that lead to these painful episodes, enabling individuals to make lifestyle adjustments aimed at prevention. Awareness of triggers is a powerful tool in the management of migraines.
The duration of stabbing head pains can also differ. Some individuals may experience episodic migraines lasting for hours, while others may suffer from more persistent chronic migraines, which can be debilitating over extended periods. Understanding these variations can provide crucial insights into the severity of the condition and inform treatment approaches tailored to the individual.
Ultimately, gaining a comprehensive understanding of stabbing head pains is the first step toward effective relief and prevention strategies. Recognizing the symptoms, triggers, and variations in pain intensity provides a foundation for patients to engage in more informed discussions with healthcare providers about their treatment options.
Effective Relief Strategies for Migraine Sufferers
For many individuals suffering from chronic migraines, immediate pain relief is paramount. Over-the-counter medications like ibuprofen and acetaminophen can be effective for milder episodes, but they do not address the underlying issues faced by chronic migraine sufferers. Prescription medications, including triptans, often provide more effective relief, especially when taken at the onset of a migraine.
Non-pharmacological approaches also play a vital role in pain relief. Techniques such as applying cold compresses to the forehead or using relaxation exercises can help alleviate pain during an episode. Many individuals find biofeedback and meditation beneficial, as these strategies promote relaxation and can reduce stress, a common trigger for migraines.
Other relief strategies include acupuncture and chiropractic care, which may release tension and improve overall well-being. While scientific evidence supporting these therapies varies, many patients report subjective improvement from these alternative treatment options. Exploring these methods can offer additional tools in one's migraine management arsenal.
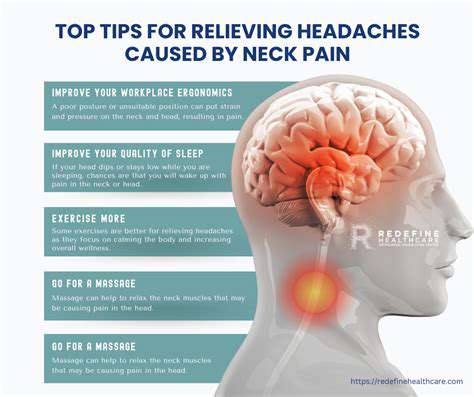
Additionally, lifestyle changes can significantly contribute to pain relief. Regular exercise has been shown to reduce headache frequency and severity, while maintaining hydration and a balanced diet can help stave off migraines triggered by dietary factors. Sufficient sleep is also crucial for migraine prevention, making it essential to practice good sleep hygiene.
In summary, a holistic approach that combines pharmacological and non-pharmacological strategies is essential in managing stabbing head pains effectively. By exploring various methods, individuals can tailor their migraine relief plans to their unique needs and experiences.
Preventive Measures for Chronic Migraines
Preventive measures are vital for chronic migraine sufferers who experience frequent stabbing head pains. Identifying personal triggers through a headache diary can lead to valuable insights that guide lifestyle changes, thereby reducing the frequency of migraines. Common triggers to note include certain foods, stress levels, and environmental factors, among others.
Medications designed specifically for migraine prevention may be recommended, including beta-blockers, antidepressants, or anticonvulsants. It's crucial for individuals to have open discussions with their healthcare providers to determine which medication aligns with their personal health profiles and migraine history.
Incorporating dietary changes can also serve as a preventive strategy. Some patients find that eliminating trigger foods, such as aged cheeses, processed meats, or artificial sweeteners, significantly reduces the incidence of migraines. Creating a balanced diet, rich in whole foods, can also help improve overall health and support the body’s physiological processes.
Establishing a consistent routine is beneficial in reducing migraine attacks. Regular sleep schedules, balanced meals, and scheduled exercise can all contribute to enhanced well-being, reducing the likelihood of migraines triggered by irregularities. Mindfulness practices such as yoga and deep-breathing exercises can decrease stress, another key trigger for migraines.
Preventive strategies require an individualized approach, acknowledging that what works for one person may not work for another. Through trial and error, chronic migraine sufferers can establish a robust prevention plan tailored to their lifestyles, enhancing their quality of life and reducing the frequency of debilitating head pains.
Role of Lifestyle Changes in Migraine Management
Lifestyle changes can profoundly influence the intensity and frequency of stabbing head pains for migraine sufferers. Identifying personal triggers allows individuals to make informed lifestyle modifications tailored to their unique needs. For instance, avoiding specific foods or beverages that are known to provoke migraines can significantly decrease the likelihood of experiencing debilitating pain.
Regular physical activity is another essential lifestyle modification that promotes migraine management. Engaging in aerobic exercises has been shown to enhance overall physical health and can reduce the frequency of stabbing head pains. However, it is crucial to find a balance, as excessive strain or abrupt changes to exercise routines might serve as triggers instead.
Stress management techniques can significantly aid in migraine prevention. Incorporating relaxation practices, such as yoga or tai chi, not only helps relieve tension but also promotes mental well-being. Mindfulness meditation can cultivate a greater awareness of one’s body, allowing individuals to recognize and address early signs of an impending migraine.
Additionally, maintaining a regular hydration level is critical for migraine management. Dehydration can trigger headaches, making water intake essential. Incorporating hydrating foods into one's diet, such as fruits and vegetables, can also contribute to overall wellness while supporting optimal body function.
In the realm of sleep hygiene, establishing consistent sleep patterns plays a pivotal role in preventing stabbing head pains. Creating a soothing bedtime routine, limiting screen time before bed, and optimizing the sleep environment increase the chances of achieving restorative sleep, reducing the risk of migraine attacks triggered by sleep deprivation.
Seeking Professional Help: When to Consult a Specialist
Recognizing when to seek professional help is essential in effectively addressing stabbing head pains and finding appropriate relief. Individuals who experience frequent migraines that interfere with daily activities should consult a healthcare professional, ideally a headache specialist. A thorough examination and assessment of symptoms can lead to a tailored treatment plan that addresses personal pain experiences.
Consulting with a specialist is particularly crucial if migraines change in pattern or intensity, or if there is an unusual onset of symptoms, such as vision changes, confusion, or weakness. These signs may indicate a more severe underlying condition, so timely evaluation is vital to ensure proper care.
Healthcare professionals can provide guidance in navigating treatment options and offer recommendations for medications that cater specifically to migraine relief. They may also suggest comprehensive approaches, combining pharmacological treatments with lifestyle adjustments, ensuring a holistic response to migraine management.
In some cases, patients may also benefit from working with other specialists, such as nutritionists or physical therapists, who can address co-existing conditions or help identify dietary or physical factors contributing to migraines. This collaborative approach ensures that all aspects of a patient's health are considered in their treatment plan.
In conclusion, actively seeking professional guidance is a significant step toward managing stabbing head pains effectively. By partnering with healthcare providers and specialists, individuals can gain insights into their condition and explore diverse strategies that pave the way for improved quality of life and reduced migraine frequency.
Support and Resources
Understanding Migraine Triggers
Identifying migraine triggers is essential for those who suffer from chronic migraines. Triggers can vary greatly from person to person, making it crucial to keep a migraine diary. This diary should include potential triggers such as certain foods, environmental factors, and emotional stress levels. By understanding what specifically triggers an individual's migraines, they can start to reduce the frequency and severity of their episodes.
Common triggers can include dietary components like aged cheeses, caffeine, and processed meats. Over time, many migraine sufferers learn to avoid these specific foods, leading to an enhanced quality of life. Additionally, hormonal changes and lack of sleep can significantly affect the onset of migraines, emphasizing the importance of a stable routine that prioritizes good sleep hygiene and stress management.
Environmental factors such as bright lights, loud noises, or strong smells can also serve as triggers. For this reason, finding and creating a comfortable living space is vital. For those who work in bustling environments, utilizing tools like noise-canceling headphones or wearing sunglasses indoors can help mitigate these environmental triggers and lessen the likelihood of a migraine attack.
Lastly, it is worthwhile to analyze emotional health as a trigger for migraines. Stress and anxiety often go hand in hand with chronic migraines, contributing to a vicious cycle. Techniques such as mindfulness meditation, yoga, and regular physical exercise can help manage emotional well-being and could ultimately lessen the frequency of migraine attacks.
Professional Support Networks
Seeking professional help is an important step in managing chronic migraines. Healthcare providers such as neurologists, headache specialists, and primary care physicians can offer valuable insights and treatment options tailored to individual needs. Regular consultations can help patients find the right medication and therapeutic strategies needed to alleviate their debilitating head pain.
In addition to traditional medical professionals, support groups can be an invaluable resource for chronic migraine sufferers. Connecting with others who share similar experiences provides emotional support, practical coping strategies, and useful information on new treatment alternatives. Many associations, such as the National Headache Foundation, offer resources and forums to help individuals engage with others navigating similar challenges.
Physical therapists specializing in migraines can also play a crucial role in the support network. They can design personalized exercise and stretching regimens aimed at alleviating muscular tension that may contribute to migraines. Furthermore, techniques like manual therapy or acupuncture have shown promise in reducing migraine frequency for some individuals.
Finally, psychological counseling or cognitive-behavioral therapy can provide essential support for managing chronic pain. Mental health professionals can equip sufferers with coping strategies to address the depression or anxiety often related to chronic migraines. This holistic approach to treatment allows for both physical and mental aspects of migraine management to be addressed effectively.
Resources for Self-Management
Self-management techniques are crucial for chronic migraine sufferers seeking relief. Many resources, including apps designed to track migraine occurrences, can help individuals pinpoint triggers and understand the patterns related to their attacks. Popular apps often feature built-in reminders for medication, hydration, sleep schedules, and strategies for mindfulness—all essential factors in effective migraine management.
Educating oneself about migraines can also empower sufferers in their journey. Various websites and publications focus on migraine education, advocacy, and research. Understanding the condition helps patients recognize that they are not alone in their struggle and fosters a sense of community among chronic migraine sufferers.
Integrating lifestyle changes can make a noticeable difference in the frequency of migraines. Factors such as diet, hydration, routine exercise, and sleep can significantly contribute to overall wellbeing. Resources like meal plan guides tailored for migraine sufferers can provide useful insights on how dietary changes impact symptom management.
Finally, many self-help books and wellness programs focus on natural and holistic approaches to migraine relief. These resources may delve into topics like herbal supplements, aromatherapy, and nutrition tailored specifically for migraine management. Exploring various self-help avenues allows sufferers to find effective strategies that resonate with their personal journey.