Decoding Migraine Symptoms: Beyond Just Head Pain
Headache Variations: From Throbbing to Pressure
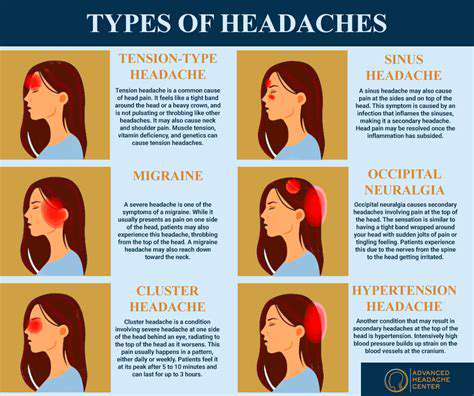
Understanding Tension Headaches
Nearly everyone experiences tension headaches at some point—that persistent, dull ache wrapping around your skull like an invisible vise. Unlike their more dramatic cousins, these headaches creep in subtly, often triggered by everyday stressors: looming deadlines, poor ergonomics at your workstation, or even that third cup of coffee you shouldn't have had. What makes them particularly insidious is how easily we dismiss them as normal, when in reality they're our body's distress signals.
Combatting tension headaches requires a multi-pronged approach. Try setting phone reminders to correct your posture every hour, or experiment with progressive muscle relaxation techniques during lunch breaks. The real game-changer comes from recognizing patterns—keeping a simple headache diary can reveal surprising triggers, whether it's that afternoon chocolate bar or your monthly budget meeting.
Migraine Headaches: A Different Beast
Imagine your head suddenly transforming into a construction zone—jackhammers pounding behind one eye, fluorescent lights feeling like daggers, and even the hum of your refrigerator becoming unbearable. This is migraine territory, where pain isn't just a symptom but a full-body experience. The peculiar prodrome phase often begins hours before the pain hits, with subtle warnings like unexplained yawning, food cravings, or sudden mood shifts that most sufferers only recognize in hindsight.
Modern migraine management has evolved beyond just painkillers. Neurologists now recommend migraine hygiene—consistent sleep patterns, hydration tracking apps, and identifying trigger foods through elimination diets. Emerging research shows promise with non-pharmaceutical interventions, like applying ice packs to the neck during attacks or using green-tinted glasses to reduce light sensitivity.
Cluster Headaches: A Short, Intense Episode
Dubbed suicide headaches by medical professionals, cluster headaches deliver pain so severe it's been compared to childbirth or kidney stones—except it's concentrated around one eye. Victims often pace relentlessly during attacks, as lying down worsens the agony. These headaches follow bizarrely precise biological clocks, frequently striking at the same time each day or appearing seasonally when daylight hours change.
Recent breakthroughs in treatment include high-flow oxygen therapy and nerve stimulation devices. What's fascinating is how cluster headaches correlate with nicotine use—many sufferers report their first attack shortly after quitting smoking. This paradoxical relationship continues to puzzle researchers studying the condition's complex neurovascular mechanisms.
Rebound Headaches: A Potential Side Effect
Here's the cruel irony—the very medications meant to relieve headaches can spawn new ones when overused. Rebound headaches create a vicious cycle where each dose provides diminishing relief while making your brain more pain-sensitive. Most people don't realize they're trapped in this cycle until they try skipping their usual dose and experience withdrawal symptoms worse than the original headache.
Breaking free requires careful tapering under medical supervision, often replacing painkillers with alternative therapies. Some headache specialists prescribe short courses of steroids to bridge the withdrawal period. The silver lining? Most patients report dramatic improvement within weeks of breaking the medication cycle, though the process requires patience and support.
Other Types and Considerations
Headaches can originate from surprising sources—a misaligned jaw, inflamed sinuses, or even referred pain from neck vertebrae. Cervicogenic headaches, for instance, stem from cervical spine issues but manifest as forehead pain. Dentists increasingly collaborate with neurologists when TMJ disorders trigger chronic head pain.
Environmental factors play underappreciated roles. Barometric pressure changes affect some people like human barometers, while others react to perfumes or cleaning product fumes. Creating a headache-safe environment at home and work—with proper lighting, ergonomic setups, and air purifiers—can yield unexpected benefits for chronic sufferers.
Beyond the Head: Accompanying Symptoms
Beyond the Throbbing: Understanding Associated Symptoms
Migraine symptoms extend far beyond head pain, creating what neurologists call the migraine experience. Some patients develop temporary speech difficulties or tingling sensations that mimic stroke symptoms, leading to unnecessary ER visits. These neurological fireworks reflect the condition's complex impact on brain function.
Visual Disturbances: Seeing Beyond the Pain
Aura symptoms can resemble avant-garde art—scintillating scotomas that look like shimmering fortresses or zigzag patterns expanding across your visual field. Some migraineurs experience Alice in Wonderland syndrome, where objects appear distorted in size or distance. These phenomena stem from cortical spreading depression, a wave of altered brain activity that marches across the cortex.
Sensory Sensitivity: A World in Discomfort
During attacks, ordinary stimuli become weapons—the refrigerator's hum morphs into a bass drum, sunlight feels like sandpaper on retinas. Some sufferers report osmophobia, where normally pleasant smells like coffee or perfume trigger nausea. This hypersensitivity originates from thalamic dysfunction, the brain's sensory gatekeeper going haywire.
Nausea and Vomiting: Unwanted Companions
Migraine-related nausea differs from typical stomach upset—it's a neurological nausea that persists even with an empty stomach. Some patients discover unexpected relief from unconventional remedies like sniffing alcohol wipes or acupressure wristbands. The gut-brain connection in migraines has led researchers to investigate probiotics and gut microbiome therapies.
Cognitive Impairment: Brain Fog and Difficulty
Migraine brain resembles trying to think through molasses—words escape mid-sentence, simple calculations become impossible, and focusing feels like tuning a staticky radio. Some patients experience postdrome for days after pain subsides, jokingly calling it their migraine hangover. These cognitive symptoms correlate with altered cerebral blood flow patterns visible on specialized MRI scans.
Emotional Fluctuations: Mood Swings and Emotional Distress
The emotional rollercoaster includes pre-attack irritability (prodrome rage), mid-attack despair, and post-attack euphoria. Some patients report sudden crying spells or anxiety attacks hours before pain begins. This emotional component suggests limbic system involvement, with the amygdala becoming hyperactive during attacks.
Other Associated Symptoms: A Spectrum of Experiences
Lesser-known symptoms include allodynia (pain from harmless touches), temperature dysregulation, and even unilateral nasal congestion. Some patients develop food cravings—particularly for chocolate or salty foods—during prodrome. These diverse manifestations underscore why migraine is considered a neurological disorder rather than just a headache condition.