Effective Strategies for Managing Occipital Neuralgia Pain
What is Occipital Neuralgia?
Understanding Occipital Neuralgia
Occipital neuralgia is a type of headache that occurs when the occipital nerves, located at the back of the head, become inflamed or injured. This condition often manifests as sharp, shooting pain that can radiate from the base of the skull to behind the eyes, which can be both debilitating and difficult to manage.
The pain is typically unilateral, meaning it often affects only one side of the head. Patients may also experience other symptoms such as sensitivity to light, neck stiffness, and even occasional areas of tenderness along the scalp. Understanding these symptoms is crucial for early diagnosis and treatment.
Occipital neuralgia can be caused by various factors, including head injuries, muscle tension, or underlying health conditions such as arthritis. Identifying the underlying cause of the pain is essential for effective management and developing a tailored treatment strategy.
Diagnosis of Occipital Neuralgia
Diagnosing occipital neuralgia often begins with a thorough medical history and physical examination. Healthcare providers may perform specific tests to assess the nerves involved and determine the potential causes of the pain. This may include neurological assessments or imaging studies like MRI scans.
It's important for patients to provide detailed information about their symptoms, including the nature, duration, and triggers of their pain. This information can help healthcare providers distinguish occipital neuralgia from other headache types, such as migraines or tension headaches.
In some cases, a nerve block may be performed as a diagnostic tool. If the injection of anesthetic provides significant pain relief, it further confirms the diagnosis of occipital neuralgia and can guide future treatments.
Treatment Options for Occipital Neuralgia
Managing occipital neuralgia typically involves a multi-faceted approach that may include medications, physical therapy, and lifestyle changes. Over-the-counter pain relievers such as NSAIDs can help alleviate mild symptoms, while prescription medications, such as muscle relaxants or nerve blocks, may be necessary for more severe pain.
Physical therapy is another important aspect of treatment. Targeted exercises can help improve neck strength and reduce muscle tightness, potentially relieving pressure on the occipital nerves. Heat therapy or massage may also offer additional symptom relief.
In some cases, more invasive procedures such as nerve decompression surgery or occipital nerve stimulation may be recommended. These options are typically considered when conservative treatments fail to provide adequate relief.
Lifestyle Adjustments and Pain Management Techniques
Patients can also benefit from certain lifestyle adjustments to help manage their occipital neuralgia pain. Maintaining proper posture, particularly for those who spend long hours at a computer, can help reduce strain on the neck and prevent exacerbation of symptoms.
Incorporating stress management techniques such as mindfulness, yoga, or meditation into one's daily routine can also help mitigate pain. Chronic pain can often be exacerbated by stress; thus, finding ways to relax and reduce tension is vital.
Finally, keeping a headache diary can be an effective strategy to identify triggers and patterns associated with occipital neuralgia. Documenting factors such as diet, sleep, and activity levels allows patients and their healthcare providers to create a more personalized and effective pain management plan.
Common Symptoms and Causes
Understanding Occipital Neuralgia Symptoms
Occipital neuralgia is characterized by sharp, shooting pain that typically begins at the base of the skull and can radiate to the scalp, forehead, and behind the eyes. Many individuals describe this pain as similar to an electric shock or a severe headache.
Some common symptoms accompanying the pain include sensitivity to light, tenderness in the scalp, and discomfort when touching the neck or back of the head. These symptoms can be debilitating and significantly impact daily activities.
Additionally, episodes of pain may be triggered by specific movements of the neck, certain postures, or even prolonged periods of resting the head in one position. Identifying these triggers can be crucial in managing symptoms effectively.
In some cases, individuals might experience a sensation of a dull ache that persists in between sharper periods of pain, contributing to ongoing discomfort and affecting overall quality of life.
It is essential to recognize these symptoms early, as timely intervention can often lead to more effective management and relief from the pain associated with occipital neuralgia.
Identifying Common Causes of Occipital Neuralgia
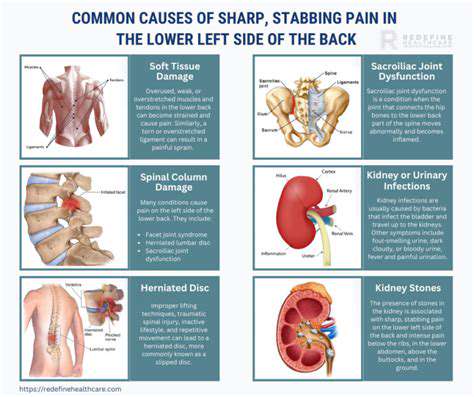
Occipital neuralgia can arise from various underlying causes, with the most prevalent being irritation or injury to the occipital nerves. This can occur due to trauma, muscle tension, or conditions such as arthritis or herniated discs.
Muscle tension and spasms in the neck may lead to compression of the occipital nerves, contributing to the onset of pain. This tension can often be exacerbated by poor posture or ergonomic issues, especially for those who spend extended periods at a desk.
Other potential causes include infections, such as shingles, that impact the nerves, or systemic conditions like diabetes, which can lead to nerve damage. Recognizing these causes can help guide appropriate treatment options.
In some instances, the cause of occipital neuralgia may be idiopathic, meaning the specific reason for nerve irritation is unclear. This can complicate diagnosis and management strategies for affected individuals.
Understanding the diverse range of causes is crucial for healthcare providers to tailor treatments effectively, thereby offering relief to individuals suffering from occipital neuralgia.
Effective Pain Management Techniques
Managing occipital neuralgia pain often requires a multifaceted approach, and individuals are encouraged to work closely with healthcare professionals to find the best strategies for their specific situation. One of the primary methods is the use of medications, which may include anti-inflammatory drugs, muscle relaxants, or nerve block injections.
Physical therapy can also play a significant role in pain management. Exercises targeting neck strength and flexibility, combined with techniques like massage, can help reduce muscle tension and improve overall neck health.
Heat or cold therapy is another effective strategy. Applying a warm compress or an ice pack to the affected area can provide quick relief for some individuals, helping to soothe nagging pain and reduce inflammation.
For chronic cases, alternative treatments such as acupuncture or chiropractic adjustments may offer additional relief. These holistic approaches can target nerve pathways and alleviate pain without reliance on pharmaceuticals.
Lastly, lifestyle modifications, including stress management techniques and regular exercise, can enhance overall well-being and help mitigate the frequency and intensity of occipital neuralgia episodes.
When to Seek Medical Help
While some degree of discomfort may be manageable at home, it is vital to recognize when to seek medical assistance for occipital neuralgia. If pain becomes severe, persistent, or accompanied by other neurological symptoms such as blurred vision or weakness, immediate medical attention is essential.
A healthcare provider can conduct thorough assessments, including physical examinations and imaging tests, to identify any underlying conditions that may require more specialized treatment.
Regular consultations with a healthcare professional can help monitor the condition and adjust treatment plans as necessary. This proactive approach enables individuals to stay ahead of their pain management strategies.
Additionally, if over-the-counter pain relief is ineffective, or if side effects are troublesome from prescribed medications, discussing alternative options with a healthcare provider is critical.
Finally, mental health support may also be beneficial, as chronic pain can lead to anxiety and depression. Addressing these emotional aspects is an integral part of comprehensive pain management for individuals with occipital neuralgia.
Diagnosis of Occipital Neuralgia
Understanding Occipital Neuralgia Symptoms
Occipital neuralgia is characterized by sharp, jabbing pain that often begins at the base of the skull and can radiate towards the forehead, temples, or behind the eyes. This pain, which can be debilitating, is frequently accompanied by tenderness in the scalp and neck area. Patients may also experience sensitivity to light and an increased discomfort when making specific head movements.
Other symptoms that accompany occipital neuralgia may include chronic headaches, usually described as a throbbing or pulsating sensation. Some individuals report experiencing pain that mimics migraines, making it difficult to differentiate between the two conditions without proper medical evaluation. In some cases, this pain can occur intermittently or be continuous, worsening with certain activities or stress.
Recognizing these symptoms promptly is crucial for diagnosis and treatment. Individuals suffering from these signs should consult a healthcare professional for a thorough assessment. Early diagnosis often leads to more effective pain management strategies, minimizing the impact of the condition on everyday life.
Diagnostic Techniques for Occipital Neuralgia
Diagnosing occipital neuralgia typically begins with a comprehensive medical history and physical examination performed by a healthcare provider. This may involve discussing the patient's pain characteristics, triggers, and any previous treatments attempted. The clarity of symptoms assists in narrowing down the potential causes of the pain.
In some cases, imaging studies such as MRI or CT scans may be utilized to rule out other potential sources of headaches or neck pain. These scans can help identify conditions like herniated discs or tumors that might be contributing to nerve irritation. Additionally, nerve blocks may be used as both a diagnostic tool and a therapeutic approach to understand the source of the pain.
Accurate diagnosis is essential, as it informs the subsequent management plan and helps prevent unnecessary treatments. Collaborating with neurologists and pain specialists may enhance the diagnostic process, ensuring a holistic evaluation of the patient’s condition.
Treatment Options for Occipital Neuralgia
Managing occipital neuralgia often involves a combination of medication and non-invasive treatments. Over-the-counter pain relievers, muscle relaxants, and anti-inflammatory drugs are frequently prescribed to alleviate acute pain attacks. In more severe cases, healthcare providers may recommend prescription medications, including anticonvulsants or antidepressants, which have shown efficacy in managing nerve-related pain.
In conjunction with pharmacological treatments, physical therapy can prove beneficial for patients by strengthening neck muscles and improving posture. Targeted exercises, stretching, and manual therapy techniques may alleviate tension around the occipital nerves, reducing the frequency and intensity of pain episodes.
For individuals who do not respond to conservative treatments, more invasive options such as nerve blocks, steroid injections, or neuromodulation techniques (like occipital nerve stimulators) may be considered. These treatments aim to interrupt the pain signals transmitted through the affected nerves, offering longer-lasting relief for chronic conditions.
Lifestyle Adjustments for Pain Management
Adopting certain lifestyle changes can significantly improve the management of occipital neuralgia. Maintaining good posture, especially during long periods of sitting or working at a computer, can reduce unnecessary strain on the neck and occipital region. Ergonomic adjustments in the workplace, including proper chair height and monitor placement, may mitigate discomfort.
Implementing stress-reduction techniques, such as mindfulness, yoga, or meditation, can help manage headaches and associated pain. Regular physical activity not only improves overall health but also aids in reducing muscle tension in the neck and shoulders, potentially alleviating some symptoms of occipital neuralgia.
Additionally, establishing a consistent sleep routine can play a crucial role in pain management. Ensuring adequate sleep quality and quantity helps the body recover, may decrease pain sensitivity, and enhance one's ability to cope with chronic pain conditions. Keeping a headache diary can also help identify triggers that could be avoided.
Effective Pain Management Strategies

Understanding Occipital Neuralgia
Occipital neuralgia is characterized by sharp, stabbing pains that originate in the back of the head or neck and travel up the scalp. It's often caused by irritation or injury to the occipital nerves, which can result in severe headaches. Identifying the specific triggers of these pain episodes is crucial for effective management.
Common triggers include neck tension, repetitive neck movements, and poor posture. Understanding how these factors contribute to the condition can empower individuals to make lifestyle changes that alleviate symptoms. Furthermore, consulting with healthcare professionals can help create a tailored approach to treatment.
Education about the condition enables individuals to better navigate their pain management options and discuss them with healthcare providers. Incorporating this knowledge can enhance communication and lead to more effective treatments.
Non-Pharmacological Treatments
Non-pharmacological treatments play a significant role in managing occipital neuralgia. These approaches may include physical therapy, which focuses on stretching and strengthening neck muscles to reduce pain. Incorporating daily exercises can help improve posture and alleviate tension, thus decreasing the frequency of pain episodes.
Other methods such as acupuncture have also shown promise in providing relief. By stimulating certain points in the body, acupuncture may help to relieve pain and promote relaxation, creating a holistic approach to treatment.
Additionally, mindfulness and relaxation techniques, like meditation or yoga, can contribute to overall well-being. Establishing a routine that incorporates these practices may reduce stress, which can be beneficial for managing pain levels.
Medications and Medical Interventions
In some cases, medication may be necessary to manage the pain associated with occipital neuralgia. Common options include NSAIDs, muscle relaxants, and nerve blocks, which can provide temporary relief from acute episodes. It's essential to work closely with a healthcare provider to find the most effective medication regimen.
For individuals who do not respond to conventional treatments, more invasive options might be considered. These can include occipital nerve stimulation, a procedure that involves placing a small device near the occipital nerves to block pain signals.
Before pursuing any medical intervention, a thorough consultation and assessment are necessary. Understanding the potential risks and benefits of various treatments can help patients make informed decisions about their pain management strategies.
Lifestyle Changes to Alleviate Pain
Making specific lifestyle adjustments can significantly impact the management of occipital neuralgia. For instance, maintaining proper posture while sitting and working can reduce strain on the neck and help minimize pain triggers. Incorporating ergonomic furniture and tools can make a substantial difference in everyday comfort.
Additionally, staying hydrated and following a balanced diet can support overall health, potentially providing some relief from pain symptoms. Implementing regular sleep routines can also improve sleep quality, which is often affected by chronic pain.
Finally, engaging in stress-reduction activities, such as hobbies or socializing, can help improve emotional well-being. A positive mental state can influence the perception of pain and contribute to better overall management.
When to Seek Medical Help
Understanding the Symptoms
Occipital neuralgia is characterized by sharp, shooting pain that radiates from the back of the head and down the neck. Many individuals describe the pain as similar to an electric shock, often exacerbated by neck movement or prolonged positions. It's important to differentiate this condition from other headaches, as the localized nature of the pain is a key indicator of occipital neuralgia.
Other symptoms may include sensitivity to light, tenderness in the scalp, and occasional nausea. Additionally, some individuals report episodes of pain that can be triggered by activities such as coughing, sneezing, or even turning the head. Recognizing these symptoms early can lead to more effective management strategies.
If you notice consistent or escalating symptoms, it's crucial to consult a healthcare provider who can evaluate your condition and recommend appropriate treatments. Ignoring early signs may lead to increased discomfort and a longer recovery period.
Self-Care Techniques
While professional medical advice is essential, self-care can play a significant role in managing occipital neuralgia pain. Applying heat or cold to the affected area can help alleviate discomfort. A heat pack can promote blood flow, while an ice pack can reduce inflammation and numb sharp pains.
Gentle stretching and neck exercises are also beneficial in relieving tension in the muscles surrounding the occipital nerves. Activities such as yoga and physical therapy can improve flexibility and strength, potentially preventing future episodes of pain.
Additionally, maintaining a proper posture during daily activities can contribute to reducing strain on the neck. Ergonomic adjustments in your workspace and being mindful of your head and neck alignment while sitting can make a significant impact on your symptoms.
Medical Treatments and Interventions
If self-care methods prove inadequate, medical interventions may be necessary. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can provide temporary relief. However, it is important to consult a healthcare professional about the appropriate medications for your specific situation.
More advanced treatments may include nerve blocks, where an anesthetic is injected around the occipital nerve to interrupt pain signals. Physical therapy, corticosteroid injections, or even alternative treatments like acupuncture may also be recommended, depending on individual circumstances.
In severe cases, surgical options may be considered, particularly if conservative treatments fail to offer relief. Discussing these options with a qualified healthcare provider can help you weigh the potential benefits and risks of each approach.
Preventive Measures for Future Pain
Preventive strategies are key to reducing the frequency and severity of occipital neuralgia episodes. Regular exercise and maintaining a healthy lifestyle can enhance overall physical well-being, which may mitigate the likelihood of pain development. Incorporating activities that promote relaxation, such as meditation and deep-breathing exercises, can also help manage stress that might trigger pain.
Keeping track of potential headache triggers, such as specific foods, stressors, or lifestyle habits, can empower you to make informed choices. A headache diary may be useful in identifying patterns and connecting triggers to painful episodes.
Lastly, staying well-hydrated and ensuring adequate sleep can also contribute positively to pain management. Prioritizing sleep hygiene and addressing any existing sleep disorders can provide a solid foundation for both physical and mental health, further helping to control occipital neuralgia symptoms.