Exploring Vagal Nerve Stimulation (VNS) for Migraines
What is Vagal Nerve Stimulation (VNS)?
What is the Vagal Nerve?
The vagus nerve is the longest cranial nerve in the human body, playing a crucial role in numerous bodily functions. It's a complex part of the autonomic nervous system, responsible for regulating involuntary actions like heart rate, digestion, breathing, and even some aspects of mood and emotional responses. Its extensive network of branches extends throughout the body, connecting to various organs and tissues, making it a vital component of maintaining homeostasis.
Understanding the vagus nerve is fundamental to comprehending the potential benefits and mechanisms of vagal nerve stimulation (VNS). Its extensive reach and influence on a wide array of bodily systems highlight the intricate workings of the human nervous system and its role in overall well-being.
How Does VNS Work?
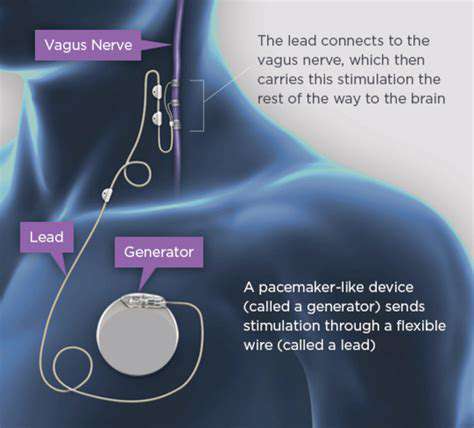
Vagal nerve stimulation (VNS) is a neurostimulation therapy that involves implanting a small device, similar to a pacemaker, under the skin. This device sends electrical impulses to the vagus nerve, aiming to modulate its activity and, consequently, the signals it transmits to the brain. The precise mechanisms by which VNS achieves its therapeutic effects are still being researched, but it's believed to influence brain activity and neurotransmitter levels, potentially impacting various neurological and mental health conditions.
The goal is to interrupt or modify the abnormal signals that might be contributing to the specific condition being treated. The hope is that the stimulation can help the brain re-establish a more balanced state.
Types of VNS Devices
Different types of VNS devices are available, each with its own specifications and functionalities. These devices are surgically implanted, with specific components designed to deliver precisely calibrated electrical pulses to the vagus nerve. The precise programming of the device is crucial to optimize its effectiveness and minimize potential side effects.
Conditions Treated with VNS
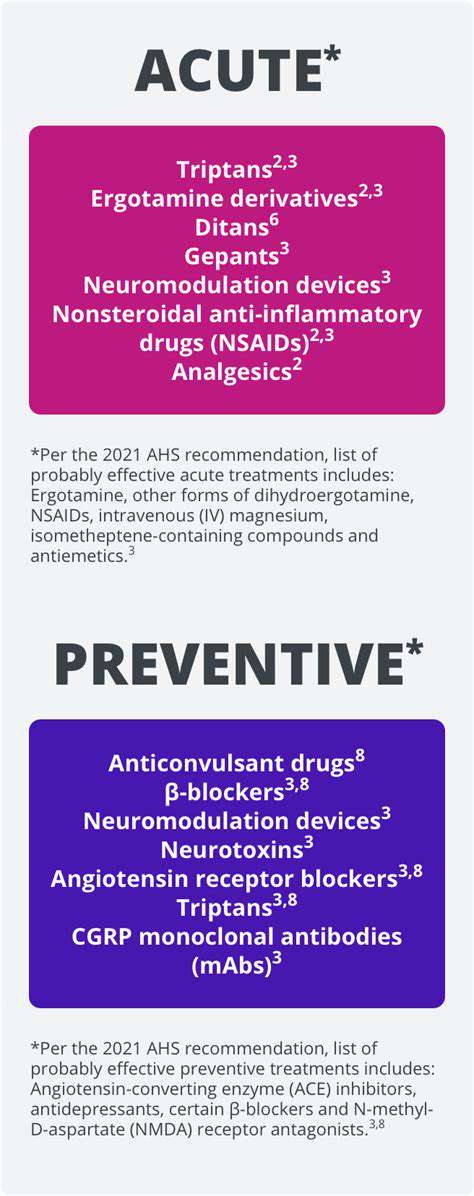
Vagal nerve stimulation (VNS) is primarily used to treat specific neurological and mental health disorders. One of the most prominent applications is in the management of treatment-resistant epilepsy, where it can help reduce seizure frequency. VNS is also being investigated for its potential in treating other conditions, including depression, anxiety, and certain types of chronic pain.
However, the effectiveness of VNS varies greatly depending on the individual and the specific condition being addressed. Thorough evaluation and careful consideration of the potential benefits and risks are essential when considering VNS as a treatment option.
Surgical Procedure for VNS
The surgical procedure for implanting a VNS device is generally performed under general anesthesia. A small incision is made, and the device is carefully positioned beneath the skin, typically in the chest area. Careful attention to surgical technique and precise placement of the device are crucial for minimizing complications and maximizing effectiveness.
Post-operative care, including medication management and follow-up appointments, is an integral part of the overall treatment process. Ongoing monitoring and adjustment of the device's settings are often necessary to optimize its therapeutic impact.
Potential Benefits and Risks
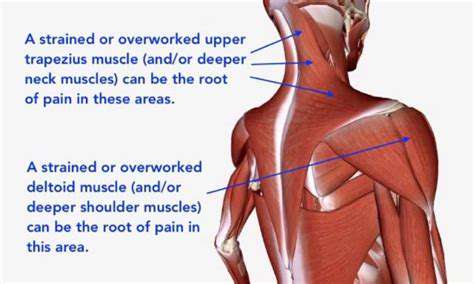
While VNS holds promise for managing various conditions, it's important to acknowledge both the potential benefits and the inherent risks. Among the potential benefits are reduced seizure frequency, improved mood regulation, and pain relief. However, potential side effects such as hoarseness, voice changes, and swallowing difficulties may occur. Furthermore, complications such as infection or device malfunction can also arise.
A thorough discussion of potential benefits and risks is essential for informed decision-making regarding VNS as a treatment option.
Long-Term Management and Follow-up
Long-term management of VNS involves regular follow-up appointments with a medical professional to monitor the device's function and evaluate its effectiveness. Adjustments to the device's settings may be necessary based on the patient's response to treatment and any emerging side effects or complications. This proactive approach ensures that the device continues to deliver optimal therapeutic benefits while minimizing potential risks.
Patient education and active participation in their care are crucial for successful long-term outcomes. Understanding the device's operation and potential side effects empowers patients to effectively manage their care and communicate any concerns to their healthcare team.