Exploring the Connection Between Stress and Chronic Pain
The Biochemical Response to Stress
The Role of Cortisol in Pain Perception
Cortisol is a steroid hormone released by the adrenal glands during times of stress. It plays a crucial role in the body’s fight-or-flight response. Chronic elevation of cortisol levels can lead to heightened sensitivity to pain. This is because cortisol has a direct impact on the nervous system, influencing pain pathways.
In conditions of prolonged stress, persistently high cortisol levels can alter pain perception, making mild sensations feel more intense. This alteration can contribute to the development of chronic pain syndromes. Understanding this relationship highlights the need for stress management in pain treatment plans.
Additionally, high cortisol levels can lead to inflammation, which is another critical factor in pain development. Inflammatory markers activated by stress can result in long-term pain issues, particularly in individuals predisposed to inflammatory disorders.
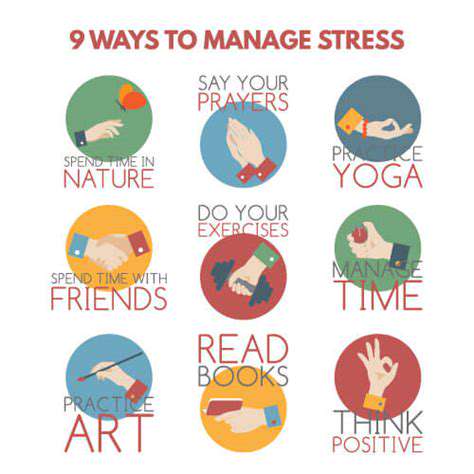
Managing cortisol through techniques like mindfulness, meditation, and physical exercise can be beneficial. Implementing these stress-reduction techniques may provide relief not only from stress but also from the chronic pain linked to it.
How Stress Affects Muscle Tension
When a person is under stress, the body naturally responds by tensing muscles. This physiological reaction can become a cycle: stress leads to muscle tension, which can subsequently cause pain and discomfort. Over time, chronic muscle tension can result in conditions such as tension headaches and neck or back pain.
Muscle tension caused by stress can lead to reduced blood flow to the affected areas, exacerbating pain and discomfort. This reduced circulation can delay recovery and increase weakness in the muscles, further aggravating the pain experienced. Recognizing this cycle is vital for effective pain management.
Stretching routines and relaxation techniques are beneficial in relieving muscle tension caused by stress. Regular physical activity can also help alleviate built-up tension, leading to reduced pain levels and improved overall function.
Furthermore, incorporating practices such as yoga or tai chi can provide dual benefits by alleviating stress and promoting muscular relaxation, thereby breaking the pain-stress cycle.
The Interplay Between Stress and Inflammation
Chronic stress is known to trigger an inflammatory response in the body, often contributing to pain exacerbation. The release of pro-inflammatory cytokines during stressful periods can lead to the development of chronic inflammatory conditions, where pain becomes a persistent companion.
Inflammation serves as a biological signal of distress but can be detrimental in conditions like arthritis or fibromyalgia, where both stress and inflammation are key components. The overlap between these factors makes understanding their interaction critical for effective management strategies.
Reducing stress through lifestyle changes, such as enhanced sleep patterns and dietary modifications, can help lower inflammatory responses. Foods rich in omega-3 fatty acids, antioxidants, and other anti-inflammatory properties can be part of a holistic approach to managing both stress and pain.
Long-term strategies to manage inflammation associated with stress may also include counseling and other therapies focused on emotional well-being, allowing individuals to break free from the stress-pain cycle while improving their quality of life.
The Psychological Impact of Chronic Pain and Stress
The relationship between chronic pain and stress can create a feedback loop where pain can lead to increased anxiety and depression, which in turn raises the perception of pain. This complex interplay necessitates a comprehensive approach to treatment that addresses both psychological and physical aspects of pain.
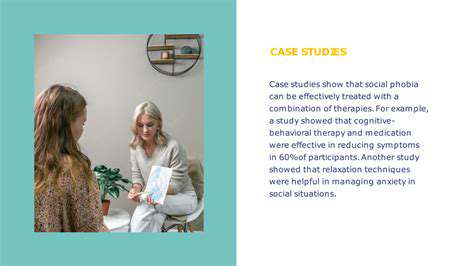
Mind-body therapies such as cognitive-behavioral therapy (CBT) can equip individuals with tools to manage the emotional distress associated with chronic pain. CBT works by altering negative thought patterns, helping people develop healthier coping mechanisms to deal with stress and pain.
Additionally, support groups can provide emotional relief and a sense of community for those suffering from chronic pain. Sharing experiences and coping strategies can help individuals feel less isolated, contributing to improved mental health.
Addressing the psychological dimension of chronic pain is essential. It can lead to enhanced treatment outcomes, creating a pathway towards improved not only physical health but also emotional resilience in the face of ongoing challenges.
Integrating Stress Management into Pain Treatment Plans
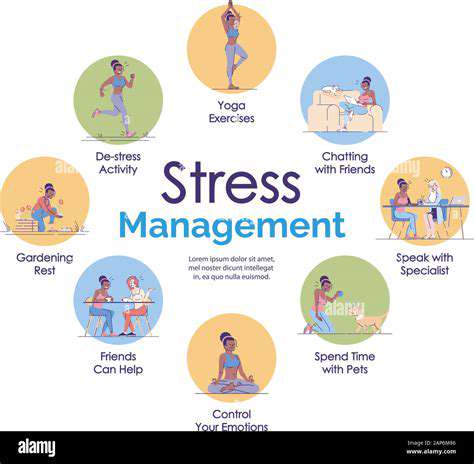
Recognizing the interconnectedness of stress and chronic pain underscores the importance of integrating stress management techniques into conventional treatment protocols. A multidisciplinary approach encompassing physical treatment, psychological support, and lifestyle modifications can yield positive outcomes for individuals living with chronic pain.
Healthcare providers can incorporate stress reduction techniques such as mindfulness training, guided imagery, and relaxation exercises as part of comprehensive pain management plans. These techniques can help lower the perception of pain while offering tools to manage stress effectively.
Patient education plays a critical role in this integrative approach. Empowering individuals to recognize stressors and their impact on pain can inspire proactive management strategies, promoting a better understanding of their health conditions.
In summary, clinical practices should prioritize a holistic view of chronic pain management. By addressing stress alongside physiological factors, healthcare providers can create more effective and supportive treatments, ultimately enhancing the overall well-being of patients.
The Mind-Body Connection

The Role of Psychological Factors
Chronic pain is often intertwined with various psychological factors, including anxiety and depression. Research indicates that these emotional states can exacerbate the perception of pain. Individuals with a history of psychological issues may experience more intense chronic pain compared to others. Understanding this connection is crucial for effective pain management strategies.
Cognitive behavioral therapy (CBT) has emerged as an effective treatment option for those suffering from both chronic pain and psychological distress. By changing negative thought patterns, CBT can help patients develop healthier coping mechanisms. This therapeutic approach not only addresses emotional wellness but also contributes to pain relief. Incorporating mental health support can significantly enhance the quality of life for patients with chronic pain.
Furthermore, mindfulness and relaxation techniques, such as meditation and yoga, have shown promise in alleviating both stress and chronic pain. These practices encourage individuals to connect with their bodies in a healing way. As patients learn to manage stress, they often report a decrease in pain levels, demonstrating the power of the mind-body connection.
In summary, addressing psychological factors is essential in understanding the complex relationship between stress and chronic pain. As treatment approaches evolve, integrating mental health strategies will be important for achieving optimal outcomes for those affected by chronic pain.
The Biological Mechanisms
The relationship between stress and chronic pain can also be explained through various biological mechanisms. Stress triggers the release of hormones such as cortisol and adrenaline, which can influence pain perception. The activation of the body's stress response system can heighten sensitivity to pain signals. This physiological response can create a vicious cycle, where pain leads to more stress, and stress exacerbates pain.
Inflammation is another key player in this connection. Chronic stress has been shown to increase inflammatory markers in the body, which can contribute to the development of chronic pain conditions. As the immune system responds to perceived threats, persistent inflammation can maintain pain even when the initial stressor has been removed.
Neuroplasticity, or the brain's ability to adapt and reorganize itself, also plays a vital role. Chronic stress can lead to changes in neural pathways that amplify pain signals. Understanding these biological processes is essential for developing targeted treatments aimed at breaking the cycle of stress and pain.
In conclusion, the biological mechanisms underlying the connection between stress and chronic pain highlight the importance of a comprehensive approach to treatment. By addressing both the psychological and physiological aspects of pain, healthcare providers can offer more effective interventions and improve patient outcomes.
Effective Strategies for Managing Stress-Related Pain
Understanding the Link Between Stress and Chronic Pain
Chronic pain and stress are often intertwined, each exacerbating the other in a cyclical manner. When a person experiences stress, the body releases hormones that can lead to muscle tension, which may increase pain sensitivity.
Moreover, the perception of pain can be influenced by emotional states. Individuals under stress may feel pain more acutely, making it crucial to address both psychological and physical components of their condition.
Relaxation Techniques for Pain Relief
One effective strategy for managing stress-related pain is the incorporation of relaxation techniques into daily routines. Practices such as deep breathing exercises, meditation, and yoga can help lower stress levels and promote muscle relaxation.
Studies have shown that regular use of these techniques can lead to a significant reduction in chronic pain symptoms, making them valuable tools in any pain management plan.
The Role of Lifestyle Changes in Pain Management
Lifestyle changes can also play a significant role in reducing stress and its impact on chronic pain. Engaging in regular physical activity, maintaining a balanced diet, and ensuring adequate sleep are all vital for overall well-being.
Furthermore, seeking support from family, friends, or professional counseling can provide emotional relief and reduce the overall burden of chronic pain and stress, fostering a healthier mindset.