Headache Sharp Pain Back of Head: What You Need to Know
Contents
- Muscle tension due to posture causes sharp pain in the back of the head.
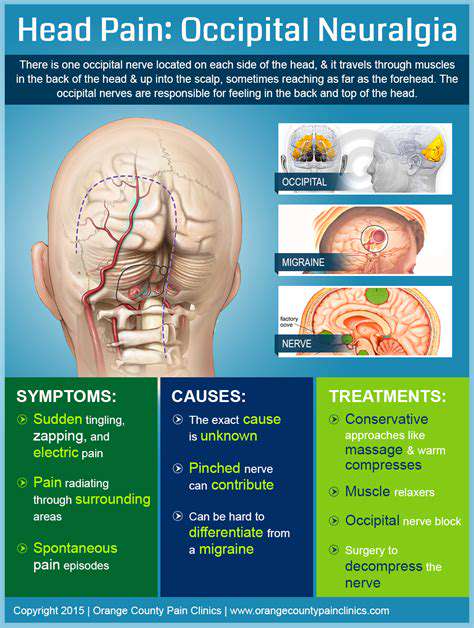
- Neurological issues like occipital neuralgia can also lead to sharp head pain.
- Symptoms include throbbing pain, neck stiffness, or nausea with severe cases.
- Conditions like migraines and cervical spine issues may cause back head pain.
- Seek medical help for sudden, severe, or unusual patterns of headache pain.
- Common misconceptions include all headaches originating from the front of the head.
- OTC medications like ibuprofen can provide relief but have potential side effects.
- Prescription medications and alternative therapies may be necessary for chronic pain.
- Regular exercise and ergonomic practices can help prevent back of head pain.
- A headache diary aids diagnosis and personalization of treatment strategies.
Common Causes of Sharp Pain in the Back of the Head
Muscle Tension and Strain
One of the most prevalent causes of sharp pain in the back of the head is muscle tension. This tension often arises from poor posture, especially when using computers or smartphones for prolonged periods. Research indicates that maintaining a forward head posture can lead to discomfort as the muscles become fatigued from trying to support the weight of the head, which can weigh around 10 to 11 pounds. This constant strain not only causes acute pain but can also lead to chronic headaches over time.
Moreover, stress and anxiety can contribute to muscle tightness, creating a vicious cycle where tension leads to pain, and pain leads to increased stress. Engaging in exercises that focus on strengthening the neck and upper back muscles, along with regular stretching routines, can alleviate this discomfort. Techniques such as yoga or Pilates can also foster better posture and resilience against tension-related pain.
Neurological Issues
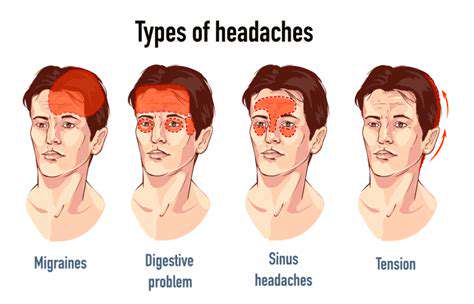
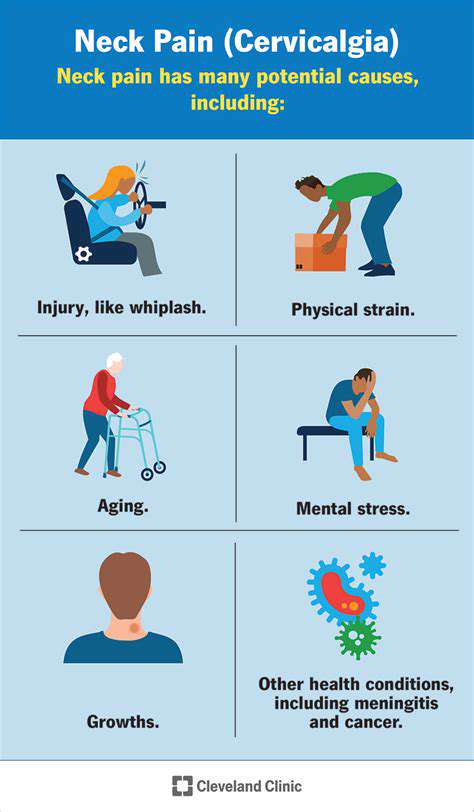
Neurological conditions such as occipital neuralgia, migraine, or cervicogenic headaches can also manifest as sharp pain in the back of the head. Occipital neuralgia, in particular, is characterized by irritation or injury to the occipital nerves, leading to sharp, jabbing pain that can radiate from the base of the skull. This condition is often mistaken for a migraine due to the nature and intensity of the pain, which emphasizes the importance of a proper diagnosis. The treatment may include medications for nerve pain, physical therapy, or nerve blocks, tailored to the individual's needs.
In terms of migraine, studies show that individuals with a history of migraines are more likely to experience similar pain patterns around the occipital region. Treatments can range from lifestyle changes to pharmaceutical interventions, making it crucial to consult with healthcare professionals who can recommend personalized strategies for managing symptoms effectively.
Symptoms Associated with Back of Head Pain
Identifying the Symptoms of Back of Head Pain
Understanding the symptoms associated with pain at the back of the head is crucial for accurate diagnosis. Typical indicators may include throbbing or sharp sensations that can fluctuate in severity. Patients frequently report a persistent, dull ache that can occasionally intensify, leading to an urgent need for relief. Tracking these symptoms is essential for both patients and healthcare providers to establish a treatment plan.
In some cases, symptoms may be accompanied by additional issues like neck stiffness or reduced mobility. This can signal underlying conditions that require immediate attention. A comprehensive symptom diary can help clarify the frequency and intensity of the pain, which can be invaluable during medical consultations.
Possible Causes of Back of Head Pain
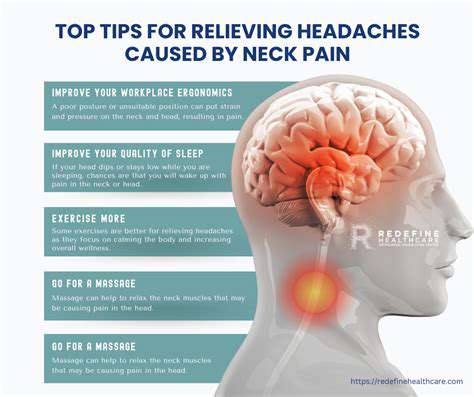
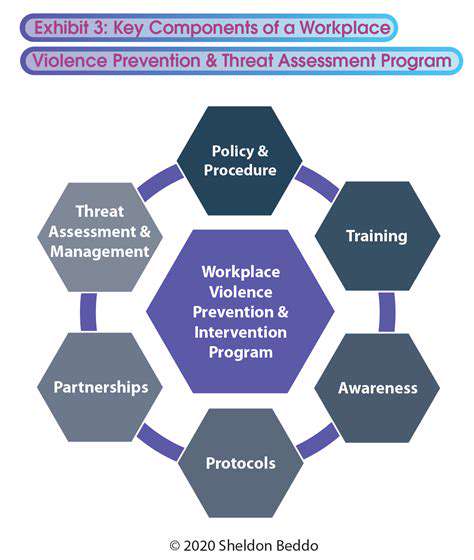
A variety of factors can contribute to pain in the back of the head. Tension headaches, for example, are often caused by stress or muscle strain, manifesting as tightness or pressure in the neck and head. Research suggests that poor posture, particularly when sitting for long periods, can exacerbate these symptoms. In fact, maintaining ergonomic practices at work and home can significantly mitigate discomfort.
Other potential causes include migraines, which, while more commonly understood to affect the temples, can also be localized at the nape of the neck. Cervical spine issues, such as herniated discs or osteoarthritis, may also lead to similar symptoms and should not be overlooked during evaluation. Knowing the range of potential causes can guide effective treatment pathways.
When to Seek Medical Attention
Recognizing when back of head pain warrants medical intervention is essential for managing health effectively. Immediate consultation is advised if the pain is severe, sudden, or differs significantly from an individual’s normal headache pattern. Signs of neurological involvement, such as vision changes or difficulty speaking, should be regarded as emergencies.
Additionally, if headaches are accompanied by other symptoms like nausea, vomiting, or high fever, these could indicate serious conditions requiring prompt evaluation. An early diagnosis can lead to better outcomes, and being aware of these red flags is a critical aspect of personal health management.
Common Misconceptions about Back of Head Pain
Many individuals harbor misunderstandings regarding back of head pain, particularly in relation to its causes and implications. A frequent myth is that all headaches originate from the front of the head; however, the nape can be just as affected due to tension and musculoskeletal issues. Adequate knowledge can dispel this myth, enabling individuals to approach their symptoms more effectively.
Another common misconception is equating all head pain with migraines. While migraines are severe and debilitating, conditions like cervicogenic headaches resulting from neck problems can produce pain in the same area but often require different treatments. Understanding these distinctions can lead to better management strategies and enhance patient outcomes.
Effective Treatments for Back of Head Pain
Treatment options for back of head pain vary depending on the underlying cause. Over-the-counter pain relievers such as ibuprofen or acetaminophen are frequently effective in managing symptoms, providing quick relief for mild to moderate pain. For conditions associated with muscle tension, muscle relaxants may also be prescribed.
In more persistent cases, physical therapy can be a beneficial avenue to explore. Stretching and strengthening exercises tailored to the cervical spine can alleviate tension and improve posture. It is often helpful to combine pharmacological and non-pharmacological treatments to achieve optimal results.
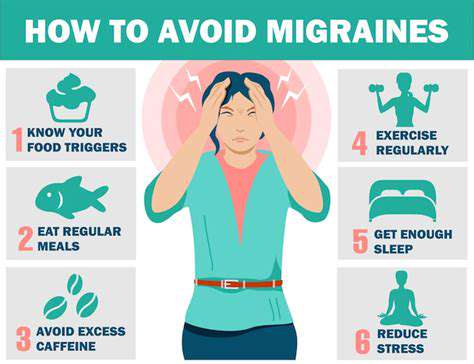
Prevention Strategies for Back of Head Pain
Taking proactive measures can significantly reduce the frequency and severity of back of head pain. Regular exercise, particularly activities that enhance neck and shoulder strength, can play a pivotal role in prevention. Incorporating stretches into daily routines can also help mitigate tension buildup that can lead to headaches.
In addition, implementing good ergonomic practices at work, such as ensuring computer screens are at eye level and using supportive chairs, can prevent posture-related issues. Mindfulness techniques and stress management can contribute to overall well-being, helping individuals cope with the triggers of tension headaches more effectively.
When to Seek Medical Attention
Identifying Severe Symptoms
When experiencing sharp pain at the back of the head, it's crucial to identify associated symptoms that may indicate a serious condition. Symptoms such as sudden vision changes, dizziness, or difficulty speaking can be concerning. An article published in the American Journal of Neurology highlights that these symptoms can be linked to conditions like a stroke or a transient ischemic attack (TIA), both of which require immediate medical intervention.
Furthermore, if the sharp pain is accompanied by nausea or vomiting, it could suggest increased intracranial pressure or meningitis. According to research from the Centers for Disease Control and Prevention (CDC), these symptoms are alarming and necessitate prompt evaluation, potentially in an Emergency Room setting.
Listening to your body is key. If the sharp pain disrupts your routine or intensifies quickly, don't hesitate to seek help. Not every headache is life-threatening, but it’s better to err on the side of caution, especially when unusual symptoms present themselves.
When to Visit the ER
There are specific scenarios where visiting an emergency room becomes essential. If the sharp pain occurs suddenly and reaches maximum intensity almost immediately, the so-called thunderclap headache, you should seek emergency care right away. This type of headache can be indicative of a potentially life-threatening condition, such as a ruptured aneurysm. The Journal of Emergency Medicine underscores the importance of timely intervention in these cases to optimize outcomes.
If you have a history of head injury, even if it feels minor, and you start experiencing sharp pain or confusion, don’t wait. Head injuries can lead to complications that might not be immediately obvious. Medical professionals can perform imaging tests to rule out damage like concussions or bleeding in the brain.
Consulting with Your Healthcare Provider
For chronic headaches that evolve into sharp pain at the back of your head, it’s advisable to schedule a visit with your primary care physician. Consistent patterns of headaches may be a sign of underlying conditions such as tension-type headaches or cervicogenic headaches stemming from cervical spine issues. Research published in the Pain Management Journal indicates that proper diagnosis and treatment are instrumental in managing chronic headache disorders effectively.
It's also wise to keep a headache diary to track patterns, severity, and triggering factors. This information can be invaluable for your healthcare provider in diagnosing the underlying cause of your pain. A personalized treatment plan based on your specific triggers can significantly improve your quality of life. Potential strategies might include physical therapy, medication, or lifestyle modifications.
Treatment Options for Pain Relief
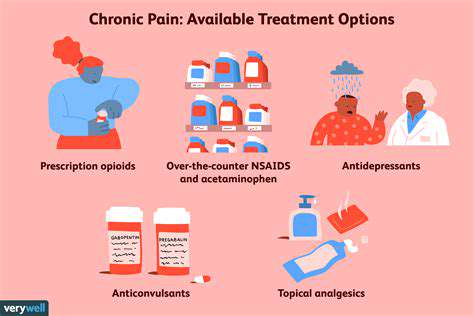
Over-the-Counter Medications
- Commonly used drugs include NSAIDs and acetaminophen.
- Always consider potential side effects and interactions.
- Consult a healthcare provider if symptoms persist.
Over-the-counter (OTC) medications are often the first line of defense against headaches. Common choices include non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin, as well as acetaminophen. These medications are effective in reducing pain and inflammation, but they also come with potential side effects. Before starting any OTC med, be sure to read the instructions and consider any pre-existing health conditions.
Many people rely on the convenience of OTC options, but it's crucial to understand their limitations. For instance, overuse can lead to rebound headaches, which can worsen your condition. It’s advisable to use these medications sparingly and consult a healthcare professional if headaches continue or worsen over time.
Prescription Medications
- Triptans are often prescribed for migraine relief.
- Preventative medications can help reduce the frequency of headaches.
- Always discuss potential risks with your doctor.
When OTC options do not provide adequate relief, it may be time to consider prescription medications. Doctors often prescribe triptans, which are designed specifically for treating migraine headaches. These medications work by stimulating serotonin receptors, thereby alleviating pain. Understanding the specific type of headache you experience is essential, as the most effective treatment can vary.
In addition to acute treatments, many individuals benefit from preventative medications. These can include beta-blockers, antidepressants, or anticonvulsants. It’s important to Find the right doctor who understands your specific needs, as this can significantly improve your quality of life. If you’re often reaching for pain relief, discussing longer-term strategies with your provider can be a game-changer.
Alternative Therapies
- Acupuncture can be beneficial for some patients.
- Physical therapy addresses underlying muscle tension.
- Mindfulness and relaxation techniques can help manage pain.
Many people seek alternative therapies for pain relief, and some have found methods like acupuncture to be particularly effective. This ancient practice involves inserting thin needles into specific points on the body, promoting circulation and balance. Evidence suggests that acupuncture may help reduce the frequency and intensity of headaches for some individuals. If you’re curious about this approach, it’s important to seek out a certified practitioner.
Physical therapy can also offer a way to relieve pain by addressing the underlying muscle tension that may contribute to headaches. Through targeted exercises and stretches, a physical therapist can help alleviate discomfort and improve overall function. Incorporating relaxation techniques, such as mindfulness meditation or yoga, can further aid in pain management by reducing stress and tension, which are common headache triggers.