Is Caffeine Helping or Hurting Your Headaches?
Neurologists describe caffeine's effect on headaches as a pharmacological paradox. For occasional users, caffeine's vasoconstrictive properties can abort migraine attacks by narrowing dilated blood vessels. But regular consumers experience the opposite effect - their brains adapt to constant caffeine by growing additional adenosine receptors, making them more susceptible to withdrawal headaches when they skip their usual dose.
This explains why the same person might find relief from a caffeine-containing painkiller during a rare headache, yet suffer daily withdrawal headaches if they typically consume multiple coffees each day. The key variable is habituation - infrequent users benefit from caffeine's acute effects, while daily drinkers become victims of their own tolerance.
The Headache-Reducing Power (and Limitations)
The Science Behind Headaches
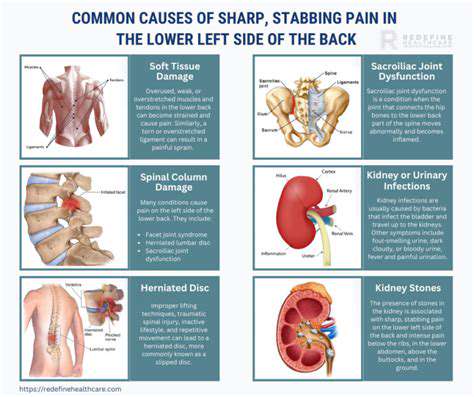
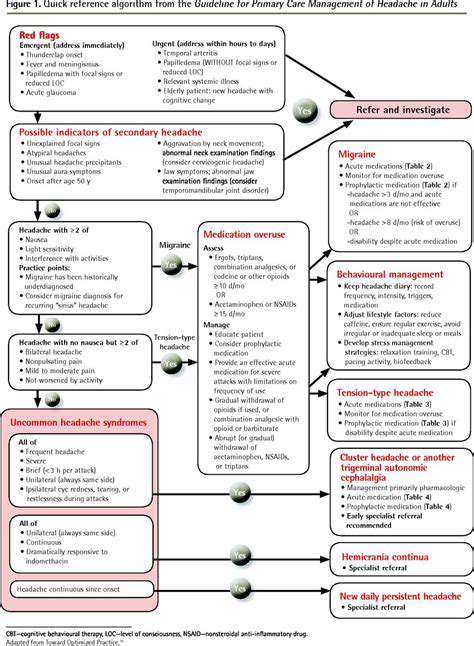
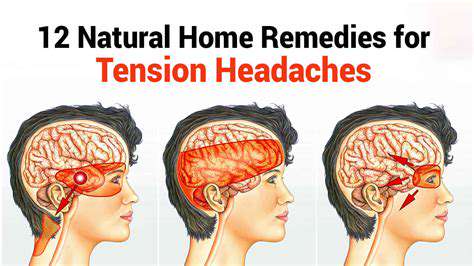
Modern neurology categorizes headaches into distinct biological pathways, each with unique triggers and mechanisms. Tension-type headaches involve overactive pericranial muscles, while migraines stem from waves of abnormal neuronal activity called cortical spreading depression. Cluster headaches, the most severe form, appear linked to hypothalamic dysfunction and trigeminal nerve activation.
Environmental triggers interact with these biological vulnerabilities in complex ways. Barometric pressure changes can trigger migraines in weather-sensitive individuals by altering intracranial pressure. Dehydration headaches occur when reduced blood volume causes the brain to temporarily shrink from the skull, stretching pain-sensitive meninges.
Lifestyle Factors and Headache Frequency
Consistency proves more valuable than intensity when modifying lifestyle factors. Maintaining stable blood sugar through regular, balanced meals prevents the vasodilation that triggers hunger headaches. Hydration needs vary dramatically by body mass and activity level - a simple urine color check (aiming for pale straw) provides better guidance than generic 8 glasses advice.
Sleep quality trumps quantity for headache prevention. Maintaining consistent bedtimes (even on weekends) regulates circadian rhythms more effectively than trying to catch up on lost sleep. The 20-20-20 rule (every 20 minutes, look 20 feet away for 20 seconds) prevents digital eye strain that commonly triggers tension headaches.
Dietary Considerations for Headache Prevention
Food triggers follow highly individual patterns that defy blanket recommendations. Aged cheeses and processed meats contain vasoactive amines that precipitate headaches in some, while others react to artificial sweeteners or MSG. Keeping a detailed food/headache diary for 30 days reveals personal patterns more reliably than elimination diets.
Caffeine moderation requires strategic planning rather than abrupt changes. Gradually replacing caffeinated drinks with half-caf alternatives over 2-3 weeks minimizes withdrawal symptoms. Timing matters equally - consuming all caffeine before noon prevents sleep disruption while maintaining daytime alertness.
The Rebound Effect: A Headache in Disguise
The Phenomenon of Rebound
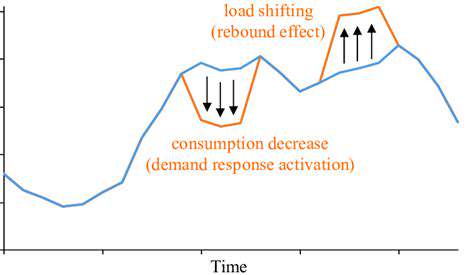
The rebound headache cycle represents one of medicine's most frustrating therapeutic paradoxes. What begins as medication providing genuine relief gradually transforms into the primary headache cause. This occurs when frequent painkiller use alters pain modulation pathways, essentially training the nervous system to expect regular analgesic input.
Breaking this cycle requires careful medical supervision. Abrupt discontinuation often worsens symptoms temporarily, while overly gradual tapering prolongs the suffering. The sweet spot involves a structured withdrawal period combined with alternative pain management strategies.
Addressing the Rebound Effect
Effective rebound management employs multiple simultaneous strategies. Preventive medications like beta-blockers or anticonvulsants help stabilize neuronal activity during withdrawal. Non-pharmacological approaches including biofeedback and physical therapy provide alternative pain modulation pathways while the nervous system resets.
Perhaps most crucially, patient education prevents recurrence. Understanding that short-term worsening leads to long-term improvement helps maintain motivation during challenging withdrawal periods. Setting realistic expectations - complete resolution may take 2-3 months - prevents premature abandonment of the treatment plan.
The hallmark of tension-type headaches isn't intensity but persistence. Unlike migraines' throbbing quality, these create a relentless vice-like pressure typically bilateral across the forehead or encircling the skull. Muscle tenderness distinguishes tension headaches from other types - pressing on trapezius or suboccipital muscles often reproduces the familiar discomfort.
Beyond the Caffeine: Addressing Underlying Issues

The Impact of Poor Sleep Hygiene
Sleep quality affects headache frequency through multiple biological pathways. During deep NREM sleep, cerebrospinal fluid flushes metabolic waste from the brain, including proteins implicated in migraine pathogenesis. Fragmented sleep disrupts this cleansing process, allowing potential headache triggers to accumulate.
Temperature regulation proves equally crucial. A bedroom temperature between 60-67°F (15-19°C) facilitates the core body temperature drop necessary for quality sleep. Overheating triggers sweating that disrupts sleep cycles, while excessive cold causes muscle tension that may precipitate morning headaches.
The Role of Stress in Energy Depletion
Chronic stress creates a perfect storm for headaches through both physiological and behavioral pathways. Elevated cortisol increases myofascial sensitivity, making muscles more prone to tension. Stress also disrupts the blood-brain barrier, allowing inflammatory compounds greater access to pain-sensitive meninges.
Effective stress management requires addressing both the stressors and the stress response. Cognitive behavioral therapy helps reframe unchangeable stressors, while regular aerobic exercise upregulates the body's endogenous opioid system for natural pain relief.
The Power of Physical Activity
Exercise's headache prevention benefits operate through multiple mechanisms. Regular aerobic activity increases pain-modulating endocannabinoids and endogenous opioids. Strength training corrects postural imbalances that contribute to cervicogenic headaches. Even gentle yoga improves proprioception, reducing the muscle misalignment that triggers tension headaches.
The key lies in finding sustainable movement patterns. Overexertion can trigger exertion headaches, while inconsistent activity fails to produce lasting benefits. A mix of cardio, strength, and flexibility work 3-5 times weekly appears optimal for headache prevention.