The Crucial Role of Symptom Awareness in Diagnosing Pain Causes
Types of Symptoms and Their Significance
Understanding Acute and Chronic Symptoms
Symptom awareness is key when distinguishing between acute and chronic pain. Acute symptoms suddenly appear and are usually a response to injury or illness. These symptoms serve as warning signals indicating that something is wrong in the body. On the other hand, chronic symptoms persist for a long time, often lasting longer than six months, and can be more complex in nature. Understanding the duration and intensity of symptoms can greatly aid in diagnosis.
Acute pain is typically sharp and intense, often leading individuals to seek immediate medical attention. In contrast, chronic pain can be more dull or aching, causing individuals to adapt their lifestyles over time. Recognizing these differences is vital for healthcare professionals. A thorough consultation about the nature of the pain can provide essential clues about the underlying causes. This awareness ultimately guides treatment decisions.
Moreover, the emotional and psychological implications of chronic symptoms should not be overlooked. Chronic pain not only affects physical health but can also significantly impact mental well-being. Those suffering from prolonged pain might face anxiety, depression, and reduced quality of life. Therefore, addressing these symptoms holistically is crucial for effective care.
It's also worth noting that the same underlying condition may manifest differently in each person. For example, an injury might trigger acute pain in one individual, while it could lead to chronic pain in another. This variability emphasizes the importance of comprehensive tracking and reporting of symptoms to doctors.
Emotional and Physical Symptoms
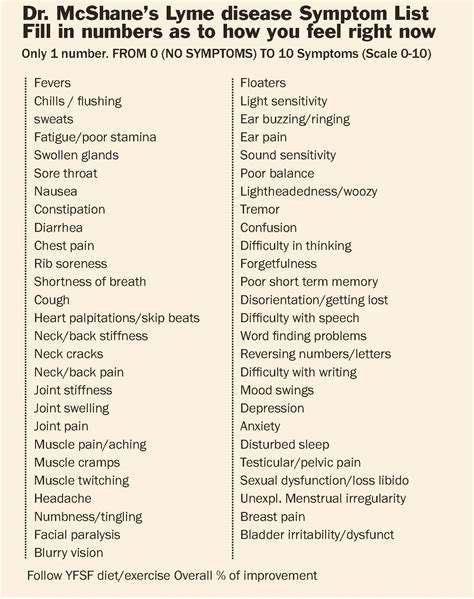
Many patients experience a mix of emotional and physical symptoms. Understanding these symptoms can enhance the diagnostic process. Both types of symptoms often intertwine, making it harder to pinpoint the exact cause of pain. Paying attention to emotional symptoms such as anxiety or depression is essential. They may provide critical insights into the pain experience.
For instance, stress can exacerbate physical pain, creating a cycle that worsens both emotional and physical well-being. Symptoms like tension headaches might signal not only a physical ailment but also an emotional burden. This dual nature of symptoms highlights the need for a comprehensive approach to diagnosis and treatment.
Some patients may be hesitant to discuss their emotional health, feeling it may be deemed less important than physical symptoms. Educating patients on the significance of these symptoms can empower them to share their full experience. Ultimately, understanding both emotional and physical symptoms leads to more personalized treatment plans.
Moreover, healthcare providers should ask probing questions that explore the relationship between pain and emotional experiences. By fostering an open dialogue, patients might feel more comfortable expressing their concerns. This openness can greatly enhance the accuracy of the diagnosis.
The Impact of Symptom Recognition on Treatment
Accurate symptom recognition can significantly affect treatment outcomes. Knowing when symptoms began, their duration, and their connection to other physical issues can help pinpoint the underlying cause. This clarity enables healthcare professionals to tailor treatments more effectively. Without this awareness, patients might receive generic treatments that don’t address their specific needs.
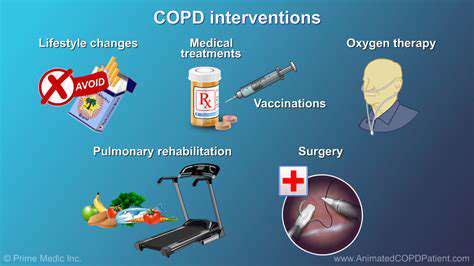
Informed discussions about symptoms allow for the exploration of multiple treatment modalities, such as physical therapy, medication, or lifestyle changes. Customized care plans can also address concurrent issues, leading to holistic health improvements. Furthermore, recognizing symptom patterns can help in monitoring the effectiveness of treatments over time.
Another crucial element is the incorporation of patient feedback into the treatment process. Regular check-ins can help identify any changes in symptoms, prompting necessary adjustments in the treatment plan. As a result, the patient remains engaged in their health journey, fostering a cooperative relationship with their provider.
Symptom awareness not only enhances individual treatment but also contributes to a better understanding of pain management broadly. As more is learned from patients' experiences, it can inform research and lead to improved therapies for various conditions.
Educating Patients on Symptom Tracking
Patient education is a vital aspect of promoting symptom awareness. Equipping individuals with tools and resources to effectively track their symptoms can greatly enhance their healthcare journey. A symptom diary, for example, can help patients note when pain occurs, its severity, and any triggering activities. Such diaries provide invaluable information during medical consultations.
Moreover, technology has made tracking symptoms easier than ever, with numerous apps available to help patients monitor their pain. These digital tools can offer reminders and visualizations, making it easier to communicate the nuances of their experience to healthcare providers. Understanding the patterns can lead to more timely interventions and appropriate treatments.
Encouraging patients to actively participate in their care empowers them and fosters a proactive approach to their health. As patients become more informed about their symptoms, they can engage in thoughtful discussions with their healthcare providers. This leads to a more collaborative approach to diagnosis and treatment.
Additionally, healthcare providers should reinforce the importance of symptom tracking during appointments, encouraging patients to bring their documentation. This ongoing dialogue can enhance trust and improve overall patient satisfaction. Through education and support, patients can become advocates for their health and make informed decisions.
The Importance of a Comprehensive Evaluation

The Multidimensional Nature of Pain
Pain is not merely a physical sensation; it is often accompanied by emotional and psychological components. Understanding the multidimensional nature of pain is crucial for accurate diagnosis and treatment. Patients may experience varying levels of discomfort due to factors such as stress, anxiety, and previous trauma, influencing their perception of pain.
Recognizing these varied dimensions can lead healthcare providers to ask the right questions during evaluations. This allows them to gather a holistic view of the patient’s experience, which can be essential for identifying the root causes of pain.
Impact of Patient History on Diagnosis
A thorough assessment of a patient's history significantly shapes the diagnostic process. Details about previous injuries, surgeries, or chronic conditions can provide insight into the current pathology. Additionally, a family's medical history can uncover genetic predispositions that may affect the patient's pain experience.
By understanding these historical contexts, physicians can narrow down potential diagnoses and tailor treatment plans to better suit individual needs. Such personalized approaches enhance the likelihood of effective pain management and improved patient outcomes.