Migraines in Women: Hormonal Influences Across the Lifespan
Menopause and Migraine: A New Chapter, New Challenges
Understanding Menopause-Related Migraine Changes
Menopause marks a significant hormonal shift in a woman's life, and this transition often brings about noticeable changes in migraine patterns. For some women, menopause can trigger new migraine episodes, while others experience a shift in existing migraine characteristics, such as frequency, intensity, or even pain location. Understanding these changes is crucial for effective management and ensuring appropriate medical interventions.
The fluctuating hormone levels during perimenopause and menopause can directly impact the trigeminal nerve, a key player in migraine pain pathways. This hormonal instability can exacerbate existing migraine triggers, making them more potent and potentially leading to more intense headaches.
Hormonal Fluctuations and Migraine Attacks
The hormonal rollercoaster during menopause is often cited as a major factor in migraine exacerbation. Estrogen, progesterone, and other hormones play a crucial role in regulating the brain's neural pathways, and fluctuations in these levels can disrupt this delicate balance, leading to more frequent and severe migraine attacks. This hormonal instability can also make it more challenging to manage existing migraine triggers, such as stress, sleep disturbances, or dietary factors.
Impact on Existing Migraine Patterns
For women already experiencing migraines, menopause can significantly alter the nature of their headaches. Some women might find that their migraines become more intense, last longer, or occur more frequently. Others might experience changes in the typical pain location, or notice new accompanying symptoms, like nausea or sensitivity to light and sound. Recognizing these changes is vital for adapting treatment strategies and ensuring optimal pain relief.
The Role of Estrogen in Migraine Prevention
Estrogen plays a complex role in migraine prevention. It's well established that estrogen has a protective effect against migraines in many women. As estrogen levels decline during menopause, this protective effect diminishes, potentially leading to a surge in migraine attacks. This understanding is crucial for developing targeted strategies to manage migraine symptoms during this life stage. Understanding the specific role estrogen plays in migraine prevention is important for women seeking tailored treatment plans.
Seeking Professional Medical Advice
Navigating menopause and migraine simultaneously can be challenging. It's essential for women experiencing these changes to seek professional medical advice. A healthcare provider can assess individual circumstances, identify potential triggers, and develop a personalized treatment plan. This plan might include lifestyle modifications, medication adjustments, or therapies aimed at managing both menopause symptoms and migraine attacks. Open communication with a healthcare professional is vital for effective migraine management during this transitional phase.
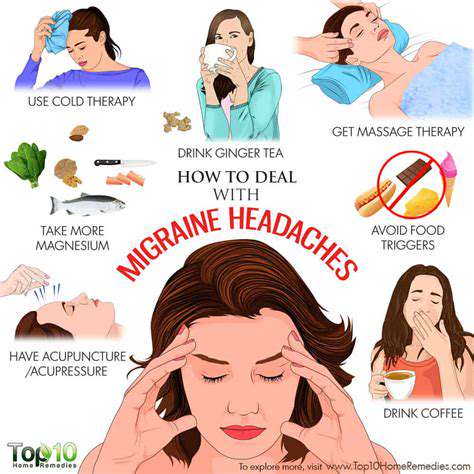
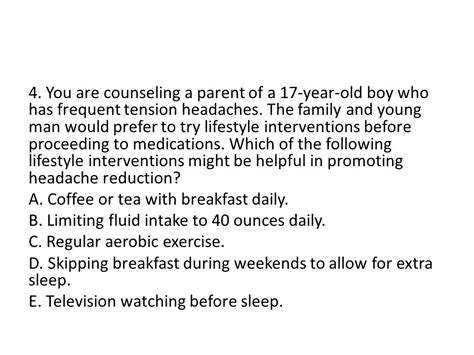
Lifestyle Modifications for Symptom Management
Beyond medical interventions, lifestyle modifications can play a significant role in managing menopause-related migraines. Strategies like stress reduction techniques, regular exercise, a balanced diet, and sufficient sleep can all contribute to reducing migraine frequency and intensity. Maintaining a healthy lifestyle, incorporating stress management techniques, and prioritizing regular sleep patterns can be invaluable tools in managing both the hormonal and migraine-related challenges of menopause.
Managing Migraines Across the Lifespan: A Holistic Approach
Understanding Migraine in Different Life Stages
Migraines can manifest differently throughout a person's life, impacting various aspects of their well-being. During childhood, migraines often present with unique symptoms, sometimes mimicking other conditions, making diagnosis challenging. Early identification and management are crucial for minimizing the impact on a child's development and overall health. Parents and caregivers should be vigilant about recognizing potential symptoms and seeking professional medical advice promptly.
As individuals move into adolescence and young adulthood, hormonal fluctuations can significantly influence migraine frequency and intensity. This period often brings about significant life changes, such as increased academic pressure, social expectations, and the potential for stress and anxiety. These factors can contribute to the exacerbation of migraines, highlighting the need for a comprehensive approach to both managing the headaches and addressing the underlying contributing stressors.
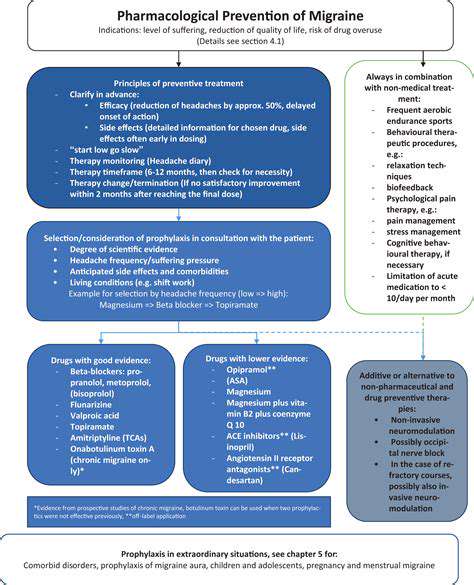
The impact of migraines can extend into adulthood and beyond, potentially affecting work, relationships, and overall quality of life. Managing chronic migraines requires a multi-faceted strategy that integrates lifestyle modifications, medication management, and stress-reduction techniques. Effective strategies for coping with migraines in adulthood often involve a combination of preventative measures and acute treatment options, tailored to the individual's specific needs and preferences.
Managing Migraines Through Different Lifestyles
Maintaining a healthy lifestyle is crucial in managing migraines across the lifespan. This includes a balanced diet rich in fruits, vegetables, and whole grains, while minimizing processed foods, caffeine, and alcohol. Regular exercise, sufficient sleep, and stress-reduction techniques, such as meditation or yoga, can all play a significant role in minimizing migraine triggers and promoting overall well-being.
Seeking support from a healthcare professional is essential for personalized guidance and management plans. A neurologist or other qualified healthcare provider can help identify potential triggers, recommend appropriate medications, and develop a comprehensive treatment strategy that accounts for individual needs and preferences. They can also provide valuable information about lifestyle adjustments and potential underlying health conditions that may be contributing to the migraines.
In addition to professional care, support groups and online resources can offer invaluable peer support and practical strategies for coping with migraines. Connecting with others who understand the challenges of living with migraines can provide emotional validation and practical advice, fostering a sense of community and shared experience.
Specific needs and circumstances related to individual lifestyles, such as work schedules, family obligations, and personal commitments, should be considered when developing a migraine management plan. Flexibility in treatment strategies is often necessary to accommodate these realities and maintain a sustainable approach to managing migraines over time.