Debunking Home Remedy Myths for Headaches
Myth Debunked: The Cooling Effect
Cold compresses have been a staple in home medicine cabinets for generations, offering relief from everything from minor headaches to sports injuries. That initial burst of coolness provides more than just surface-level comfort. Research reveals these simple tools actually trigger physiological responses that go far beyond temporary relief. When applied correctly, the cold causes blood vessels to narrow, significantly reducing both inflammation and swelling in affected areas.
This vascular constriction creates a targeted effect, temporarily limiting blood circulation to the injury site. Recognizing this localized response helps explain why cold therapy works so well for acute injuries but may not be ideal for all situations.
Understanding Inflammation
Inflammation represents the body's natural healing response, marked by telltale redness, swelling, warmth, and discomfort. Strategic cold application helps manage these symptoms by restricting blood flow to the injured area. This controlled reduction in circulation can significantly decrease discomfort while allowing the healing process to proceed more efficiently.
Clinical observations confirm that properly administered cold therapy not only reduces swelling but may actually accelerate tissue repair, potentially preventing long-term complications. While debate continues about optimal protocols, the therapeutic value of cold compresses in acute injury management remains well-documented in medical literature.
Application Techniques and Considerations
Mastering proper application methods maximizes benefits while minimizing risks. Experts recommend using commercial cold packs or ice wrapped in thin cloth - never apply frozen items directly to skin. The standard protocol suggests limiting applications to 20-minute intervals with equal periods of rest between treatments. This cycling prevents potential tissue damage while maintaining therapeutic effectiveness.
Beyond Immediate Relief: Long-Term Effects
While the immediate benefits of cold therapy are well-established, researchers continue investigating its long-term impacts. Emerging studies indicate that strategic cold application may not only reduce acute symptoms but could potentially enhance overall recovery timelines. However, medical professionals emphasize the need for more comprehensive studies to fully understand optimal treatment durations for various injury types.
Therapeutic outcomes depend heavily on multiple factors including injury severity, individual physiology, and treatment consistency. Medical guidance remains essential for developing personalized cold therapy regimens.
Precautions and Potential Risks
While generally safe when used properly, cold therapy carries risks if misapplied. Direct ice-to-skin contact can cause frostbite within minutes, while prolonged application may lead to nerve irritation. Patients should remain vigilant for unusual sensations like excessive numbness or skin discoloration, discontinuing use immediately if these occur.
Those with circulatory disorders or sensory impairments should consult healthcare providers before beginning cold therapy. Professional guidance ensures safe, effective treatment tailored to individual health circumstances.
The Role of Rest and Hydration: Essential Allies or Placebo Effects?
Rest and Recovery: Beyond the Placebo
The human body operates like a precision instrument requiring regular maintenance. Quality rest facilitates critical biological processes including cellular regeneration, hormonal balance, and neurological restoration. Decades of sleep research confirm that adequate downtime significantly impacts everything from immune response to emotional stability. For peak performance in any field - athletic, academic, or professional - prioritizing recovery should be considered non-negotiable rather than optional.
The science behind rest reveals complex physiological mechanisms often overlooked in our productivity-obsessed culture. From protein synthesis in muscle tissue to memory consolidation in the brain, recovery periods enable essential maintenance that simply can't occur during activity. Chronic sleep deprivation correlates strongly with impaired cognitive function, weakened immunity, and decreased quality of life.
Hydration: The Silent Supporter of Well-being
Water serves as the fundamental medium for all biological processes, with even mild dehydration impairing physical and mental performance. Optimal hydration maintains critical functions including thermoregulation, nutrient delivery, and toxin removal. Research demonstrates that proper fluid balance enhances concentration, endurance, and overall vitality.
Debunking the Placebo Effect: Is Rest and Hydration Truly Effective?
While the placebo effect demonstrates the power of belief in healing, the benefits of rest and hydration transcend psychological factors. Peer-reviewed studies consistently show measurable physiological improvements from proper recovery and fluid intake. These effects manifest in concrete biomarkers rather than subjective perceptions alone.
The restorative power of sleep and hydration produces objectively verifiable changes at cellular and systemic levels. These biological realities distinguish them from purely psychological interventions, making them foundational elements of health maintenance.
Rest and Hydration: Synergistic Support for Peak Performance
The combination of adequate rest and proper hydration creates multiplicative benefits for anyone pursuing excellence. For athletes, this pairing enables muscle repair, glycogen replenishment, and neurological recovery. Professionals find that strategic rest periods combined with proper hydration sustain focus and creativity throughout demanding workdays.
This powerful synergy supports sustained high performance across all domains of life, from athletic competition to creative endeavors. The combined effect often exceeds the sum of individual benefits.
Beyond Physical Benefits: The Mental Impact of Rest and Hydration
The cognitive and emotional benefits of proper recovery and hydration are equally significant as physical effects. Neurological research shows that sleep facilitates memory consolidation, emotional processing, and creative problem-solving. Conversely, dehydration reliably impairs concentration, decision-making, and mood stability.
These mental health benefits underscore why rest and hydration should be prioritized in any comprehensive wellness strategy. Their impact on quality of life and productivity makes them indispensable in our fast-paced world.

Mindfulness meditation cultivates present-moment awareness through nonjudgmental observation of thoughts and sensations, fostering deeper self-connection.
Dispelling the Ginger for Headaches Myth: A Closer Look

Dispelling the Myths
While ginger features prominently in traditional headache remedies, modern science reveals a more nuanced picture. Research suggests ginger may offer modest benefits for certain headache types due to its bioactive compounds. However, results vary significantly between individuals, and ginger shouldn't replace professional medical advice for chronic or severe headaches.
Ginger's potential value lies primarily in its anti-inflammatory compounds, which may help mitigate headache symptoms in some cases. Current evidence, while promising, doesn't support ginger as a universal headache solution. Comprehensive headache management should address underlying causes rather than relying solely on symptomatic relief.
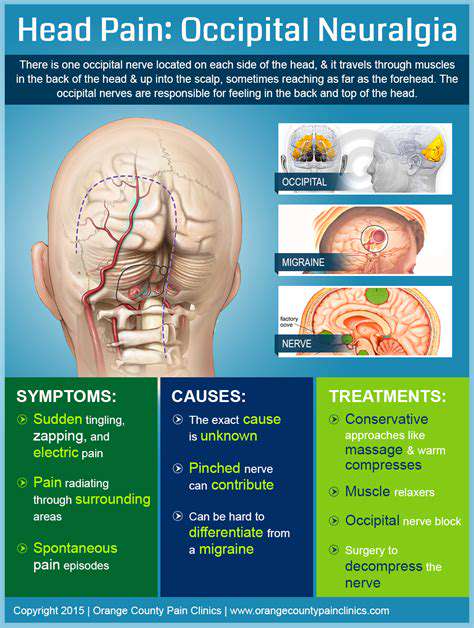
Potential Mechanisms of Action
The active components in ginger, particularly gingerols and shogaols, demonstrate anti-inflammatory and analgesic properties in laboratory studies. These compounds may interfere with pain pathways and inflammatory mediators associated with certain headache types. However, the exact mechanisms remain under investigation, with researchers exploring multiple potential pathways of action.
Scientific Evidence and Anecdotal Reports
While traditional use and anecdotal reports praise ginger's headache-relieving properties, rigorous clinical evidence remains limited. Some controlled studies show promising results for ginger in migraine management, but larger, more comprehensive trials are needed to establish definitive efficacy.
Current research indicates ginger may be most effective for certain headache types when used as part of a comprehensive treatment plan. The scientific community continues investigating optimal dosages, formulations, and treatment protocols for various headache conditions.
Important Considerations and Precautions
While generally safe, ginger can interact with blood thinners and other medications. Some individuals experience gastrointestinal discomfort, particularly at higher doses. Consultation with a healthcare provider is essential before using ginger therapeutically, especially for those with medical conditions or taking prescription medications.
Remember that headache management often requires a multifaceted approach addressing lifestyle factors, stress management, and potential underlying medical issues. Ginger may play a supportive role but shouldn't replace professional medical evaluation for persistent or severe headaches.
Beyond Home Remedies: Seeking Professional Advice
Understanding the Limitations of Home Remedies
While home treatments provide temporary symptom relief, they rarely address root causes of head and neck issues. Many popular remedies for headaches, sinus problems, and throat discomfort offer superficial comfort while potentially masking serious conditions. This delay in proper diagnosis can allow underlying issues to progress, sometimes with significant consequences. Professional evaluation ensures appropriate treatment while minimizing risks of complications.
Additionally, some home treatments can cause harm through improper use or interactions with existing medications. Healthcare providers can identify potential risks and recommend evidence-based alternatives tailored to individual health profiles.
The Importance of Accurate Diagnosis
Effective treatment begins with precise diagnosis - something home remedies simply can't provide. Medical professionals utilize physical examinations, laboratory tests, and advanced imaging to identify the true source of symptoms. This diagnostic precision enables targeted interventions rather than guesswork.
Whether dealing with bacterial infections, neurological issues, or structural abnormalities, accurate diagnosis informs appropriate treatment strategies. This level of specificity is impossible to achieve through self-treatment approaches.
Potential Risks of Self-Treatment
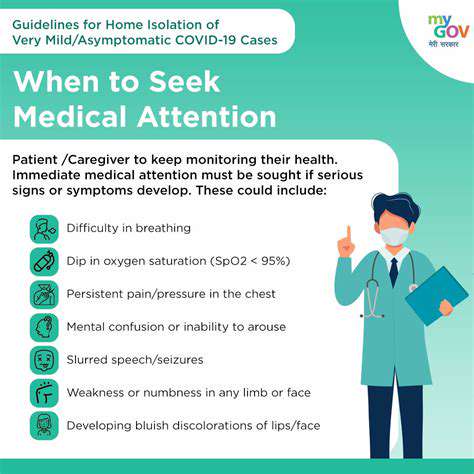
Self-managing head and neck conditions carries significant risks, particularly when symptoms indicate serious underlying issues. Delaying professional evaluation for persistent or worsening symptoms can lead to preventable complications. Additionally, unmonitored use of home remedies may interfere with prescribed treatments or existing health conditions.
Professional guidance helps navigate these risks while ensuring safe, effective treatment pathways. This is particularly important for chronic conditions requiring ongoing management.
Seeking Professional Guidance for Effective Management
Comprehensive head and neck care requires professional expertise. Healthcare providers offer complete evaluations including medical history review, physical examination, and appropriate diagnostic testing. This thorough approach enables development of personalized treatment plans addressing both symptoms and underlying causes.
Beyond acute treatment, medical professionals provide valuable guidance on prevention strategies and long-term health maintenance. Their expertise helps patients make informed decisions about when home remedies may be appropriate and when professional intervention becomes necessary.