Nerve Blocks for Headache Management: What to Know
Indications for Nerve Blocks
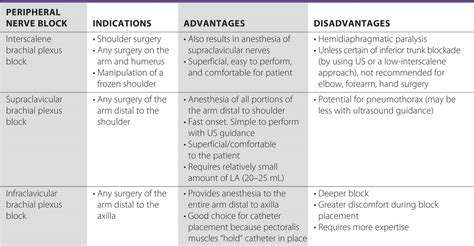
These interventions serve dual purposes—both therapeutic and diagnostic. While commonly associated with surgical pain management, their applications extend far beyond. Orthopedic specialists particularly value them for post-operative recovery, as they significantly reduce patients' need for systemic pain medications. Chronic pain management represents another critical application, offering relief when conventional treatments prove inadequate.
Procedure and Technique
Successful nerve blocks demand exceptional anatomical knowledge and technical skill. Practitioners must identify nerve locations with millimeter precision to ensure medication delivery to the intended site. Modern techniques increasingly incorporate ultrasound guidance, allowing real-time visualization of needle placement and medication spread. This technological advancement has dramatically improved success rates while reducing complication risks.
Potential Complications and Risks
Like all medical procedures, nerve blocks carry certain risks—infection, bleeding, or rare nerve injury being most notable. Meticulous sterile technique and proper patient selection form the cornerstone of risk reduction. Comprehensive pre-procedure evaluation helps identify patients who might face higher risks, while post-procedure monitoring ensures early detection of any issues.
Post-Procedure Care and Recovery
Effective recovery protocols are equally important as the procedure itself. Patients require clear instructions about expected sensations and warning signs. Establishing proper follow-up procedures ensures any concerns get addressed promptly, optimizing recovery outcomes. Most patients experience temporary numbness in the targeted area, gradually returning to normal sensation as the anesthetic wears off.
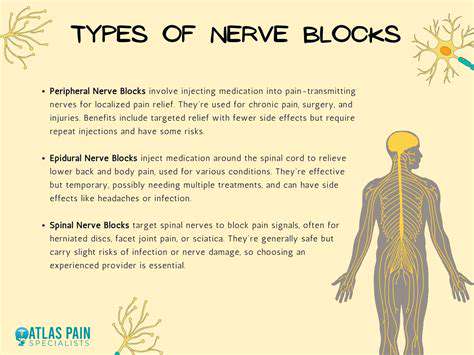
Types of Nerve Blocks for Headache Relief
Cervical Nerve Blocks
Cervical nerve blocks specifically address pain pathways originating from neck structures that often refer pain to the head. While not curative, they can provide crucial diagnostic information and temporary relief, particularly for cervicogenic headaches. The procedure typically combines local anesthetic with corticosteroids when inflammation is suspected. Patients should understand these blocks represent one component of comprehensive headache management rather than standalone solutions.
Occipital Nerve Blocks
These blocks target the greater and lesser occipital nerves, frequently implicated in tension-type headaches and occipital neuralgia. The injection site's proximity to major vascular structures demands particular precision during administration. Many patients report immediate relief, though duration varies significantly—from hours to several weeks in some cases. Combining this with physical therapy often yields superior long-term outcomes.
Sphenopalatine Ganglion Blocks
This sophisticated technique addresses cluster headaches and certain facial pain syndromes through a nerve cluster near the nasal cavity. Some practitioners employ innovative approaches like transnasal application, avoiding needle use altogether. The ganglion's complex anatomy requires specialized training for safe, effective administration. While generally well-tolerated, patients might experience temporary nasal numbness or mild bleeding.
Greater Occipital Nerve Blocks
As a primary treatment for occipital neuralgia, these blocks can dramatically improve quality of life for chronic sufferers. The technique involves identifying the nerve's exit point near the superior nuchal line—a skill requiring thorough anatomical knowledge. Many practitioners combine local anesthetic with corticosteroids to prolong therapeutic effects. Patients often report a characteristic popping sensation as the needle passes through fascial planes.
Supratrochlear and Supraorbital Nerve Blocks
These procedures target forehead pain by blocking terminal branches of the trigeminal nerve. The relatively superficial nature of these nerves makes them accessible with minimal discomfort. Precise technique is crucial as the thin eyelid skin is particularly prone to swelling. These blocks prove especially valuable for migraine patients experiencing frontal pain components.
Posterior Cervical Nerve Blocks
Addressing pain from the cervical facet joints and surrounding structures, these blocks require careful needle trajectory planning. The proximity to vertebral arteries necessitates ultrasound or fluoroscopic guidance in many cases. When performed correctly, they can provide both diagnostic information and therapeutic relief for cervicogenic headaches.
Emerging research continues to reveal concerning connections between sleep disorders and systemic health issues. The cardiovascular system appears particularly vulnerable, with sleep apnea patients demonstrating elevated risks for hypertension and related complications. These findings underscore the importance of comprehensive evaluation for patients presenting with headache complaints.
Potential Benefits and Considerations of Nerve Blocks
Therapeutic Advantages
Nerve blocks offer several distinct benefits in headache management. Their targeted nature minimizes systemic medication exposure, reducing potential side effects. For certain headache types, they can break pain cycles that prove refractory to oral medications. The diagnostic value shouldn't be underestimated—positive responses help confirm pain generators, guiding further treatment strategies.
Technical Considerations
Successful outcomes depend on multiple technical factors. Needle selection varies by target location—shorter needles for superficial nerves versus longer ones for deeper structures. Medication choice represents another critical decision point, with various local anesthetics and adjuvant medications available. Understanding pharmacokinetics helps tailor approaches to individual patient needs and desired effect durations.
Patient-Specific Factors
Not all patients make ideal candidates for nerve block procedures. Comprehensive evaluation must consider medical history, medication allergies, and bleeding risks. Patient expectations require careful management—while some experience dramatic relief, others may notice more modest benefits. Shared decision-making ensures realistic expectations and better satisfaction with outcomes.
Integration with Comprehensive Care
Nerve blocks achieve best results when incorporated into multimodal treatment plans. Combining them with physical therapy, medication management, and lifestyle modifications typically yields superior long-term outcomes. Regular follow-up allows for procedure refinement and assessment of evolving treatment needs. This comprehensive approach addresses not just symptoms but underlying contributors to headache disorders.