Tension Type Headaches: Causes, Symptoms, and Effective Management Strategies
What Causes Tension-Type Headaches?
Understanding the Triggers of Tension-Type Headaches
Tension-type headaches (TTH) can often be linked to multiple factors that contribute to their onset. One primary cause of these headaches is psychological stress, which can stem from various sources such as work, relationships, and financial pressures. When confronted with stress, the body can react physically, leading to muscle tension that manifests as head pain. Chronic stress can create a vicious cycle, where increased tension leads to more severe headaches, exacerbating the underlying stress, and perpetuating the condition.
Another significant trigger for tension-type headaches is poor posture. In our increasingly sedentary lifestyles, many individuals spend hours at desks or staring at screens, often neglecting proper ergonomics. Slouching or improper alignment can place added strain on the neck and shoulder muscles, resulting in tension that radiates towards the head, leading to discomfort. Being conscious of posture can help in preventing these headaches and making necessary adjustments to workspaces, such as using ergonomic chairs and desks.
Lack of sleep is also a commonly recognized trigger for TTH. In our fast-paced society, many people sacrifice sleep for productivity or entertainment, not realizing that insufficient rest can directly influence headache frequency and intensity. Sleep deprivation can lead to increased sensitivity to pain and heightened muscle tension, making it crucial to prioritize healthy sleep habits and create conducive sleeping environments to reduce the risk of headaches.
Dehydration is another critical factor that can contribute to tension-type headaches. When the body is not adequately hydrated, it can result in muscle cramps and tension, especially in the muscles surrounding the head and neck. Furthermore, dehydration can lead to a decrease in overall brain function, potentially magnifying headache symptoms. Staying adequately hydrated by drinking plenty of fluids throughout the day is essential in managing and preventing headaches.
Lastly, environmental factors such as excessive noise, bright lights, or unpleasant odors can also trigger tension-type headaches. These external stimuli can lead to overwhelming sensory experiences, which can cause the body to tense up and result in a headache. Identifying these environmental triggers can provide individuals with valuable information to help minimize their exposure and reduce their risk of developing tension-type headaches in various settings.
Physical and Lifestyle Factors Influencing Tension-Type Headaches
Physical factors play a pivotal role in the onset of tension-type headaches. For example, holding a certain position for an extended period, whether it's during work or leisure time, can lead to muscle fatigue and strain. Activities such as reading, gaming, or prolonged computer use can inadvertently cause individuals to strain their neck and shoulder muscles, resulting in a headache. Incorporating regular breaks and stretching exercises can significantly alleviate this issue and help maintain muscle flexibility.
Lifestyle choices, particularly regarding diet, can also influence headache occurrences. Consuming large quantities of caffeine or alcohol can result in headaches due to withdrawal symptoms or dehydration effects. Additionally, irregular meal patterns or skipping meals can lead to a dip in blood sugar levels, triggering headaches. Establishing a balanced diet that includes regular meals and a moderate intake of stimulants can be effective in headache prevention.
Moreover, the significance of regular physical activity cannot be understated in the context of preventing tension-type headaches. Exercise releases endorphins, which act as natural painkillers, helping to reduce stress and tension in the body. Activities such as yoga, stretching, or even brisk walking can help mitigate the risk of headaches. Developing a routine that incorporates movement and physical well-being can yield dramatic improvements in both mental and physical health.
Chronic medical conditions, such as anxiety and depression, can also contribute to the frequency and severity of tension-type headaches. Managing these underlying conditions through therapy, medication, or lifestyle changes can have a positive impact on headache management. Seeking professional help can provide individuals with a tailored approach to tackle both their mental health and headache issues effectively.
Finally, the importance of maintaining a healthy work-life balance cannot be overlooked. Striking a balance between professional responsibilities and personal time can significantly reduce the overall stress that contributes to headache development. Ensuring that time is allocated for relaxation, hobbies, and social interaction is crucial for mental well-being and can further aid in reducing the occurrence of tension-type headaches.
Recognizing the Symptoms of Tension-Type Headaches
Understanding the Nature of Tension-Type Headaches
Tension-Type Headaches (TTH) are among the most common form of headaches that people experience. They are characterized by a dull, pressing pain that can feel like a tight band around the head. The intensity of the pain can vary from mild to moderate, but it rarely becomes debilitating. Recognizing the specific characteristics of TTH is crucial for effective self-management and treatment.
These headaches can occur episodically or become chronic over time. Episodic TTH might present itself a few times a month, while chronic TTH can occur on 15 or more days each month. In either case, understanding the onset and duration can help individuals address the symptoms effectively. By identifying the distinguishing features of TTH, individuals can seek appropriate care sooner.
Stress, poor posture, and muscle tension are significant contributors to the development of TTH. Emotional factors may also exacerbate the condition, leading to increased frequency and intensity. Incorporating relaxation techniques and posture correction exercises can help mitigate the impact of these contributors on headache occurrence.
Moreover, recognizing that TTH symptoms can vary from person to person is essential for individualized treatment. Some may experience accompanying symptoms like mild sensitivity to light or sound, while others may not. Keeping a headache diary detailing frequency, intensity, and triggering factors can offer insights into personal headache patterns and triggers.
Identifying Triggers That Lead to Tension-Type Headaches
Identifying triggers that provoke Tension-Type Headaches can significantly improve a person's quality of life. Common triggers include stressful situations, long hours of computer work, or physical strain from exercise. Individuals often overlook these triggers, the recognition of which is essential for implementing preventive strategies. Understanding personal triggers is the first step towards adopting effective coping mechanisms.
Environmental factors such as noise, light, or even strong smells can provoke TTH in certain individuals. It’s crucial for individuals to monitor their surroundings and recognize these environmental triggers. Adapting the work environment to reduce exposure to potential stressors can play a key role in decreasing headache occurrences.
Additionally, lifestyle choices, such as poor sleep habits or dehydration, can exacerbate TTH. Keeping a consistent sleep schedule and ensuring adequate hydration throughout the day can help reduce the likelihood of headaches. Simple adjustments in daily routines often have profound effects on headache management.
Finally, hormonal fluctuations, particularly in women, are known to trigger TTH, especially related to their menstrual cycle. By tracking these hormonal changes, women can anticipate headache occurrences and prepare accordingly. This can include scheduling relaxation time or seeking medical advice if headaches become frequent during certain periods.
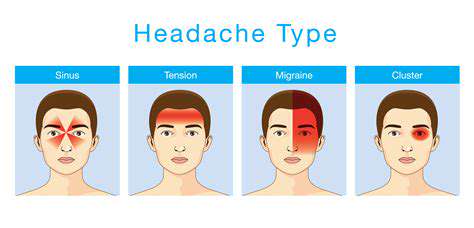
Distinguishing Tension-Type Headaches from Other Types
It's crucial to differentiate Tension-Type Headaches from migraines and cluster headaches, as each type requires distinct management approaches. Unlike migraines, TTH typically lacks the debilitating symptoms of nausea and vomiting. The pain associated with TTH is usually bilateral and doesn't exhibit the throbbing quality often found in migraine attacks.
Cluster headaches, another type of headache, are characterized by intense, piercing pain on one side of the head, often accompanying other symptoms like nasal congestion or tearing. Recognizing these differences can prevent misdiagnosis and ensure that individuals receive the most effective treatment. Understanding the nuances of each headache type is integral to implementing the correct management strategies.
Because TTH can be easily misconstrued as other types of headaches, keeping a record of symptoms is essential. Noting specific characteristics such as the duration, pain quality, and associated symptoms can help healthcare professionals make a more accurate diagnosis. This informed approach leads to more tailored and effective management plans.
Healthcare professionals often utilize this information to establish the best course of intervention, which might include medication, lifestyle changes, or even physical therapy. Education about the different types of headaches empowers individuals to take charge of their pain management. By understanding the distinctions between headaches, patients can better communicate their experiences to healthcare providers.
Effective Management Strategies for Tension-Type Headaches
Managing Tension-Type Headaches effectively involves a multi-faceted approach, combining medical treatment with lifestyle modifications. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are often the first line of defense for headache relief. However, reliance on medication should be balanced with non-pharmacological strategies to avoid rebound headaches.
Non-pharmacological approaches include stress management techniques such as yoga, meditation, or biofeedback. These practices promote relaxation and reduce muscle tension, ultimately contributing to a lower frequency of headaches. Incorporating these strategies into daily routines can empower individuals to take an active role in their headache management.
Physical therapy can also be beneficial, especially for those whose TTH is related to neck or shoulder tension. Stretching exercises, massage, and posture improvement can alleviate muscle tightness and reduce headache frequency. A well-rounded approach involving physical therapy aids in minimizing the underlying causes of tension headaches.
Lastly, developing a robust support network can play a crucial role in managing Tension-Type Headaches. Joining support groups or seeking therapy can provide emotional support and coping strategies. The shared experiences of others can often lead to discovering new management techniques that might prove effective.
Effective Management and Treatment Strategies
Understanding Tension-Type Headaches
Tension-type headaches (TTH) are among the most common headache disorders, often characterized by a constant, pressing or tightening sensation. Unlike migraines, TTH does not usually present with nausea or sensitivity to light and sound, making it crucial for individuals to recognize symptoms specific to this condition. Understanding the nature of TTH can empower patients to seek appropriate treatment and management strategies effectively.
The early recognition of tension-type headaches allows patients to mitigate their impact on daily activities. This requires a foundational understanding of potential triggers, such as stress, fatigue, and poor posture. By identifying these factors, individuals can develop targeted strategies to alleviate the frequency and intensity of headaches, thus improving their quality of life.
Effective Non-Pharmacological Treatment Options
Non-pharmacological strategies are imperative for managing tension-type headaches, especially for those seeking alternatives to medication. Techniques such as cognitive-behavioral therapy (CBT) have been shown to help patients identify and reform negative thought patterns that contribute to headache stress. Moreover, engaging in regular mindfulness practices can significantly reduce the frequency and severity of headaches.
Physical therapies, including massage and physical therapy, can target muscle tension and improve overall posture. Patients are often advised to incorporate stretching exercises or yoga into their routines, which not only alleviate existing pain but also prevent future occurrences. As these non-invasive approaches gain popularity, they offer promising benefits without the side effects associated with traditional medications.
Pharmacological Approaches to Treatment
When non-pharmacological measures are insufficient, pharmacological interventions may be necessary to manage tension-type headaches effectively. Over-the-counter pain relievers such as ibuprofen or acetaminophen are commonly recommended to reduce pain. For more chronic sufferers, healthcare providers might prescribe preventive medications that aim to decrease the frequency of headache episodes.
It is critical for patients to work closely with their healthcare providers to determine the most suitable medication, taking into account their unique medical history and potential side effects. A tailored pharmaceutical approach can significantly enhance the management of tension-type headaches, allowing individuals to maintain optimal functioning in their daily lives.
Long-term Management and Lifestyle Modifications
Long-term management of tension-type headaches significantly benefits from lifestyle modifications that promote overall health and well-being. Regular exercise, a balanced diet, and adequate hydration can play pivotal roles in reducing headache frequency. Additionally, establishing a consistent sleep schedule enhances restorative processes that can prevent headache onset.
Incorporating stress management techniques, such as yoga, meditation, or breathing exercises, can effectively lower tension levels, which are often precursors to headaches. Individuals who prioritize self-care routines and are vigilant about their triggers are more likely to enjoy a substantial decrease in the impact of tension-type headaches on their lives.