The Link Between Allergies, Sinus Issues, and Migraines
Sinus Infections and Their Impact
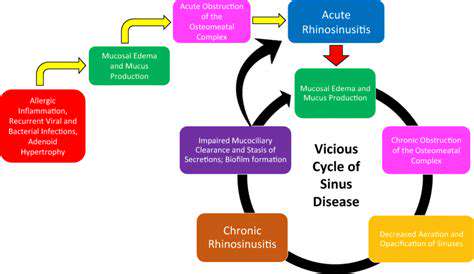
Sinus infections, commonly known as sinusitis, plague millions globally. This condition involves inflamed mucous membranes in the sinuses, triggering diverse uncomfortable symptoms. Grasping root causes and potential complications proves vital for proper treatment and prevention. Symptoms vary from mild annoyance to debilitating pain, often disrupting daily routines.
These small air pockets in our skulls connect intricately with nasal passages. When infection strikes, normal mucus flow falters, causing congestion, pressure, and discomfort. This imbalance may weaken immune defenses, increasing vulnerability to other health concerns.
Root Causes Behind Sinus Infections
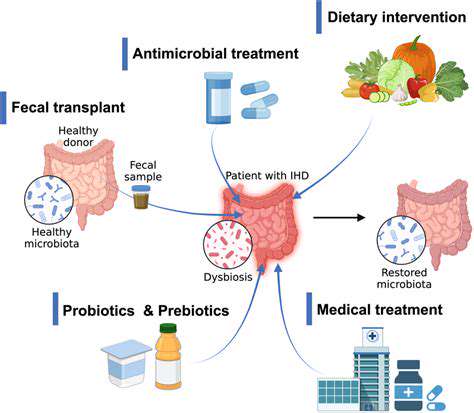
Multiple factors contribute to sinusitis development. Seasonal allergies frequently trigger inflammatory responses that block sinus passages. Viral infections like colds often precede bacterial sinusitis, creating a dangerous progression. Physical abnormalities - nasal polyps or deviated septums - may obstruct proper drainage, elevating infection risks.
Environmental elements also influence susceptibility. Smoke, dust, and pollutants can inflame tissues while weakening immune responses. Inadequate hygiene practices, particularly insufficient handwashing, facilitate pathogen transmission.
Diagnostic Methods and Treatment Options
Physicians typically diagnose sinusitis through physical exams and symptom reviews. Advanced imaging like CT scans might assess infection severity and identify structural concerns. Successful management usually combines rest, hydration, and OTC pain medication. Bacterial cases may require antibiotic prescriptions.
Supportive therapies including saline irrigation and humidifiers often ease symptoms and improve drainage. When conventional treatments fail, surgical correction of structural issues may become necessary.
Complications and Preventive Measures
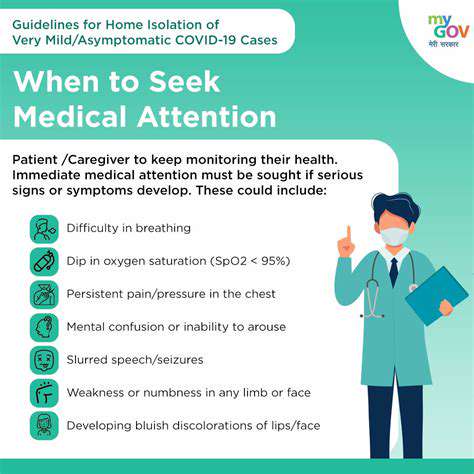
Neglected sinus infections risk serious complications, from meningitis to scar tissue formation that worsens drainage. Timely intervention remains critical to prevent these dangerous developments. Maintaining robust health through balanced nutrition and regular exercise strengthens immunity against infections.
Consistent hygiene practices - frequent handwashing and avoiding sick contacts - significantly reduce infection risks. Effectively managing underlying conditions like allergies helps prevent recurrent sinus issues.
The Allergic Trigger for Migraines
Understanding the Connection
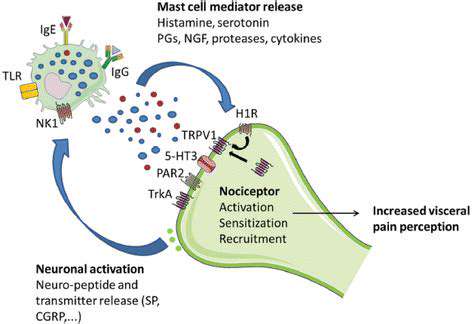
Many migraine sufferers report concurrent sinus issues and suspect allergy links. While direct causation remains unclear, research reveals complex interactions between allergic responses, sinus inflammation, and neurological migraine pathways. Allergen exposure can initiate biochemical cascades culminating in headache pain.
Allergens' Impact
Pollen, dust mites, mold, and certain foods trigger immune responses involving histamine release and inflammation. This causes nasal and sinus swelling that may generate pressure interpreted as migraine pain. The inflammatory cascade also affects the trigeminal nerve, directly involved in migraine mechanisms.
Sinus-Migraine Interactions
Sinus infections (frequently allergy-related) create substantial facial pressure that stimulates surrounding nerves, particularly the trigeminal nerve. This inflammation establishes a discomfort cycle that may trigger or exacerbate migraines.
Trigeminal Nerve's Crucial Role
This nerve serves as the primary connection between allergies, sinus issues, and migraines. Responsible for facial sensation transmission, it becomes hypersensitive during allergic inflammation, increasing migraine likelihood.
Management Approaches
Identifying personal migraine triggers through allergy testing and symptom tracking proves essential. Preventive measures include air purifiers, pollen masks, and environmental controls. OTC medications help manage symptoms, while severe cases require professional treatment plans.
Cold compresses offer therapeutic relief by reducing swelling and pain through localized cooling. Various materials work effectively, from commercial gel packs to improvised frozen vegetable wraps.