The Link Between Irritable Bowel Syndrome (IBS) and Migraines
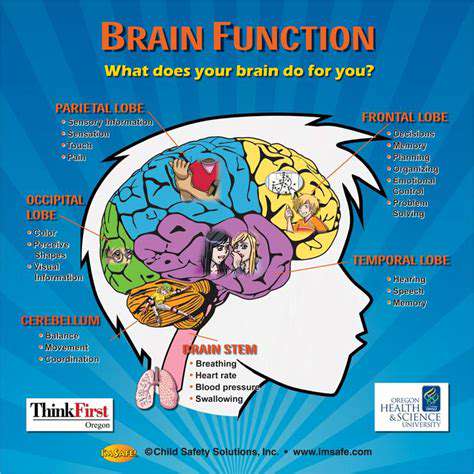
Shared Neurological Pathways in the Brain
The human brain's intricate network, with its complex web of interconnected pathways, plays a pivotal role in how we perceive and process information. Deciphering these pathways is essential for understanding the root causes of various conditions, including irritable bowel syndrome (IBS). Emerging studies indicate that overlapping neural circuits might explain why IBS patients often experience both digestive discomfort and emotional distress simultaneously. This discovery sheds light on why abdominal pain, bloating, and mood disturbances frequently coexist in IBS sufferers.
Research reveals that certain brain regions responsible for gut function and emotional regulation share neural connections. This overlap could clarify why IBS patients commonly report anxiety or depression alongside their physical symptoms. The proximity of these regions allows for a continuous feedback loop—where stress alters gut motility and sensitivity, while gut discomfort amplifies emotional distress. This bidirectional relationship underscores the profound mind-body connection in IBS.
Potential Mechanisms and Implications
Deeper investigation into these shared pathways may uncover precise biological mechanisms linking emotional states to IBS symptoms. Pinpointing the neurotransmitters and hormones involved could pave the way for innovative treatments that target both physical and psychological aspects of IBS. Such breakthroughs might revolutionize IBS management by offering personalized therapies tailored to individual neurological profiles.
The implications extend beyond IBS. Similar brain-gut interactions likely influence other conditions where psychological and physical symptoms intertwine, potentially transforming how we approach holistic healthcare. While more research is needed to map specific brain regions and neurochemicals involved, the potential benefits—from improved diagnostics to enhanced patient outcomes—are substantial.
Identifying triggers that activate these shared pathways could lead to more effective interventions. Future treatments might combine gut-directed therapies with psychological support, offering patients a comprehensive approach to managing their condition. This dual-focused strategy could empower individuals to regain control over both their physical and emotional well-being.
The Gut-Brain Axis: A Complex Interplay
The Gut Microbiome's Role
The gut microbiome—a diverse community of trillions of microbes—serves as a key communicator along the gut-brain axis. These microorganisms influence everything from nutrient absorption to immune responses and even emotional states. When this microbial balance is disrupted (a condition called dysbiosis), it may contribute to neurological and psychiatric conditions, demonstrating the profound gut-brain connection.
Certain gut bacteria can directly signal the brain via the vagus nerve or by releasing neuroactive compounds into the bloodstream. These signals can alter brain chemistry, potentially triggering mood changes or cognitive symptoms. Scientists are actively exploring how microbial metabolites interact with the immune system and nervous system to shape brain health.
The Impact of Diet on the Gut-Brain Axis
Dietary patterns significantly shape the gut microbiome and its communication with the brain. Processed foods and excessive sugars can promote dysbiosis, while fiber-rich whole foods and fermented products support microbial diversity. Simple dietary changes may therefore offer a practical way to influence both gut and brain health.
Fermented foods like yogurt and kimchi introduce beneficial probiotics that could positively impact the gut-brain axis through multiple mechanisms—from producing neurotransmitters to reducing inflammation. Ongoing research continues to identify which dietary strategies most effectively support this critical connection.
Inflammation and the Gut-Brain Connection
Chronic gut inflammation can trigger body-wide inflammatory responses that reach the brain. Inflammatory molecules called cytokines may then contribute to mood disorders or cognitive changes. Managing gut inflammation through dietary and lifestyle interventions could therefore benefit both digestive and mental health.
Stress and the Gut-Brain Axis
The stress-gut connection operates as a two-way street. Prolonged stress disrupts gut microbial balance and increases intestinal permeability, while gut disturbances can amplify stress responses. The hypothalamic-pituitary-adrenal (HPA) axis—the body's stress response system—plays a central role in this vicious cycle. Effective stress management techniques may help break this cycle and improve IBS symptoms.
The Role of Irritable Bowel Syndrome (IBS)
IBS exemplifies the gut-brain axis in action. The condition's hallmark symptoms—abdominal pain, bloating, and altered bowel habits—are often exacerbated by stress and emotional distress. This explains why many IBS patients benefit from therapies that address both gastrointestinal function and psychological well-being. A comprehensive treatment approach that considers both physical and emotional factors tends to yield the best outcomes for IBS management.
Mindfulness practice emphasizes present-moment awareness without judgment. This technique teaches individuals to observe thoughts and emotions rather than reacting to them. Developing this skill can dramatically improve emotional regulation and mental clarity.
Potential Treatments and Management Strategies
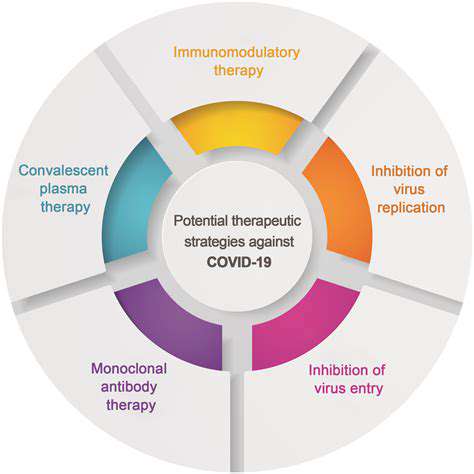
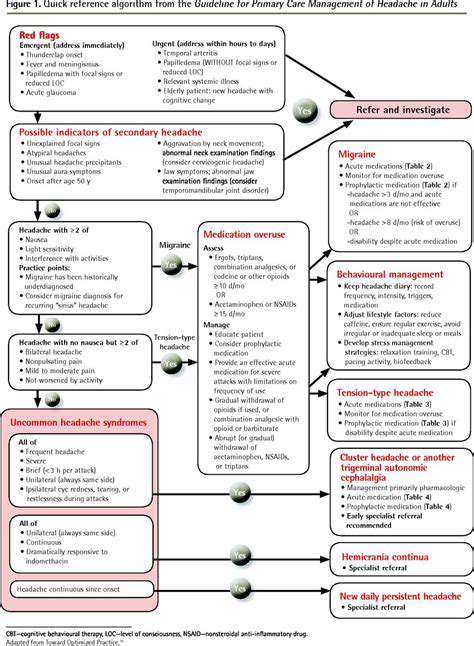
Pharmacological Interventions
Various medications target different aspects of the condition, from symptom relief to addressing underlying causes. Drugs like NSAIDs provide pain relief, while DMARDs may slow disease progression by modulating immune responses. Treatment selection depends on individual factors including symptom severity, overall health, and medication tolerance.
Physical Therapy and Rehabilitation
Customized physical therapy programs help restore mobility and reduce discomfort. Targeted exercises improve joint function while minimizing injury risk. Occupational therapy adaptations can further enhance daily functioning and independence.
Lifestyle Modifications
Weight management, balanced nutrition, and regular physical activity form the foundation of self-care. Stress-reduction techniques and quality sleep complement these efforts to support overall well-being.
Surgical Interventions
For advanced cases, surgical options like joint replacement can restore function when conservative treatments prove insufficient. These decisions require careful consideration of risks versus potential benefits.
Complementary and Alternative Therapies
While some patients find relief through acupuncture or herbal remedies, these approaches should complement—not replace—evidence-based treatments under professional guidance.
Assistive Devices and Support Systems
Mobility aids and peer support groups can significantly improve quality of life by enhancing independence and providing emotional support.
Patient Education and Self-Management
Empowering patients with knowledge about their condition leads to better outcomes. Understanding warning signs, treatment options, and self-care strategies enables individuals to actively participate in their healthcare journey.
The Importance of a Comprehensive Approach
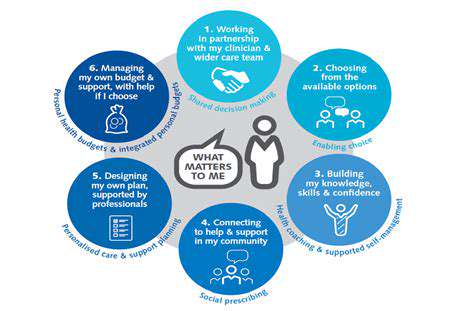
The Foundation of a Strong Strategy
Successful outcomes require considering all relevant factors rather than isolated components. Recognizing how different elements interact creates more effective solutions.
Defining the Scope
Clear problem definition through thorough research establishes a solid foundation for planning. Comprehensive data gathering ensures no critical factors are overlooked.
Measurable Objectives
Establishing concrete, trackable goals enables progress evaluation and necessary adjustments.
Implementation Planning
Detailed action plans with assigned responsibilities translate strategy into results. Effective communication ensures team alignment.
Ongoing Evaluation
Regular progress reviews allow for timely course corrections in dynamic environments.
Continuous Improvement
Analyzing outcomes provides insights for refining future strategies. This learning process drives long-term success.