What is Allodynia in Migraine? When Touch Becomes Painful
The central nervous system (CNS) is the command center of the body, responsible for processing information and coordinating responses. It's composed of the brain and spinal cord, both of which are highly complex structures containing billions of neurons. These neurons communicate with each other through intricate networks of synapses, enabling rapid and precise information transfer. The CNS interprets sensory input and initiates appropriate motor responses, ensuring the body's smooth functioning.
Peripheral Nervous System: The Body's Network
The peripheral nervous system (PNS) acts as a vast network of nerves extending throughout the body, connecting the CNS to the rest of the organism. This network carries sensory information from the environment and internal organs to the CNS for processing. It also transmits motor commands from the CNS to muscles and glands, controlling movement and various bodily functions. The PNS is crucial for interaction with the external world and maintaining homeostasis.
Sensory Input: Gathering Information
Sensory receptors throughout the body constantly monitor the internal and external environments. These receptors detect various stimuli, including light, sound, touch, temperature, and pain. They convert these stimuli into electrical signals, which are then transmitted to the CNS for interpretation. Accurate sensory input is essential for proper perception and response. This process allows us to experience the world around us and to react appropriately to changes in our surroundings.
Motor Output: Initiating Action
Once the CNS processes sensory information, it initiates appropriate motor responses. This involves transmitting signals through the PNS to muscles and glands, causing them to contract or secrete hormones, respectively. These actions enable movement, such as walking or grasping objects, as well as various physiological functions, such as digestion and hormone regulation. Motor output is crucial for interaction with the environment and maintaining the body's internal balance.
Neural Communication: The Language of the Nervous System
Neurons communicate with each other through electrochemical signals. This intricate process involves the generation and propagation of action potentials along the axon, which then release neurotransmitters at synapses. These neurotransmitters bind to receptors on the receiving neuron, triggering a response. This complex signaling mechanism allows for rapid and precise communication throughout the nervous system. Understanding these mechanisms is fundamental to comprehending how the nervous system functions and how it can be affected by various diseases and disorders. The intricate dance of electrical and chemical signals is essential for all aspects of bodily function.
Common Triggers and Manifestations of Migraine Allodynia
Common Triggers of Migraine Allodynia
Migraine allodynia, a condition where normally painless stimuli become agonizingly painful, often has complex triggers. While the precise mechanisms are still being investigated, environmental factors like bright lights, loud noises, and strong smells frequently act as potent triggers. These stimuli, which wouldn't typically cause pain in someone without migraine allodynia, can evoke a significant and debilitating response, often leading to avoidance behaviors and impacting daily life.
Furthermore, certain foods, such as aged cheeses, processed meats, and caffeine, can contribute to migraine allodynia episodes. These dietary triggers can be difficult to pinpoint as individual sensitivities vary greatly. Stress, both physical and emotional, is a significant factor. Chronic stress can exacerbate existing sensitivity to stimuli, making even minor inconveniences unbearable. Understanding these triggers is crucial for proactive management and minimizing the frequency and intensity of episodes.
Manifestations of Visual Allodynia
Visual allodynia, a type of migraine allodynia, involves heightened sensitivity to light. This can manifest as discomfort or pain from ordinary light levels, even indoor lighting. Patients often describe the experience as an overwhelming and unpleasant sensation, sometimes accompanied by throbbing or pulsating pain in the head. The intensity of the pain can fluctuate, making it challenging to predict when an episode might occur.
Beyond the visual discomfort, patients may experience photophobia, a fear or aversion to light. This can lead to avoidance of bright environments, limiting activities and social interactions. The impact on daily life can be profound, requiring adjustments to work schedules, social engagements, and even home environments.
Manifestations of Auditory Allodynia
Auditory allodynia, another form of migraine allodynia, involves heightened sensitivity to sound. This can range from mild discomfort to excruciating pain triggered by everyday noises like conversations, music, or even the sound of a ringing telephone. The intensity of the pain can vary significantly, depending on the individual and the specific sound stimulus.
The impact of auditory allodynia on daily life is substantial. Social situations, work environments, and even quiet moments at home can become sources of intense pain and distress. Avoiding potentially triggering sounds might become necessary, impacting social interactions and overall quality of life.
Manifestations of Tactile Allodynia
Tactile allodynia, a type of migraine allodynia, involves heightened sensitivity to touch. This means that even gentle or soft touches can be perceived as painful. This heightened sensitivity can manifest in various ways, from discomfort to intense pain, depending on the individual and the specific tactile stimulus.
Environmental Triggers and Their Impact
Environmental factors play a crucial role in triggering migraine allodynia. Exposure to bright lights, loud noises, and strong smells can all contribute to the development and exacerbation of migraine allodynia. These sensory triggers can vary significantly from person to person, making it challenging to pinpoint specific sensitivities.
These environmental triggers often interact with other factors, such as stress and dietary choices, to create a complex interplay that can lead to migraine episodes. Understanding these interactions is vital for effective management and prevention strategies.
Stress and Dietary Factors in Allodynia
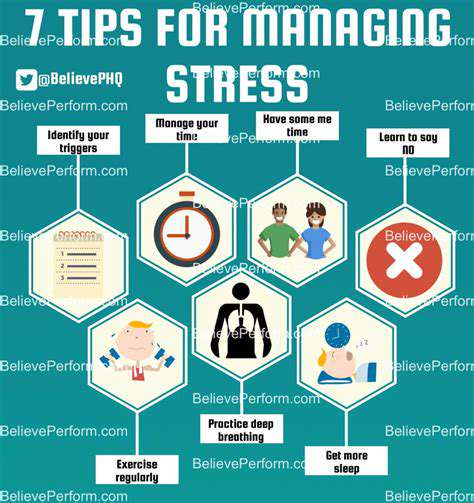
Stress, both physical and emotional, is a significant contributor to migraine allodynia. Chronic stress can exacerbate existing sensitivities to stimuli, making even minor inconveniences unbearable. The mechanisms by which stress contributes to migraine allodynia are still being investigated, but it's clear that managing stress is a crucial aspect of managing migraine symptoms.
Dietary factors can also influence migraine allodynia. Certain foods, such as aged cheeses, processed meats, and caffeine, are known to trigger episodes in some individuals. A detailed dietary history can be essential for identifying potential triggers and developing personalized management strategies.
How is Migraine Allodynia Diagnosed and Managed?
Diagnosis of Migraine Allodynia
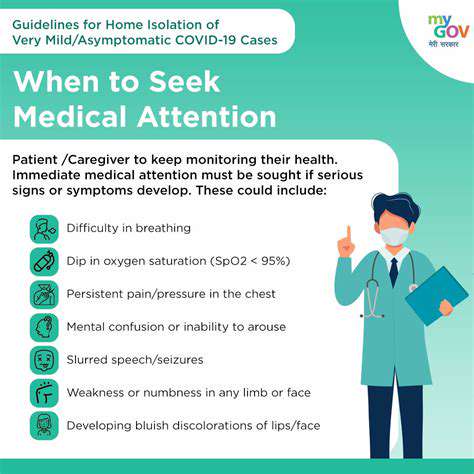
Diagnosing migraine allodynia involves a careful evaluation of the patient's symptoms, medical history, and neurological examination. A crucial aspect of diagnosis is differentiating migraine allodynia from other types of allodynia, such as those associated with nerve damage or other neurological conditions. This often requires a detailed discussion of the patient's specific triggers and pain patterns, including the location, intensity, and quality of the pain experienced. The doctor will likely ask about the frequency and duration of the pain episodes, and whether the sensitivity to touch is present only during migraine attacks or consistently.
A key diagnostic tool is a comprehensive history, meticulously documenting the patient's migraine and pain experiences. This includes the type of stimuli that provoke pain, the progression of symptoms over time, and any associated factors like stress, sleep, or environmental conditions. Neurological examinations, including sensory testing, are essential to assess the patient's sensitivity to different types of stimuli and help rule out other conditions with similar symptoms. Physicians might also employ specific diagnostic questionnaires or scales designed to quantify the severity and impact of allodynia on daily life.
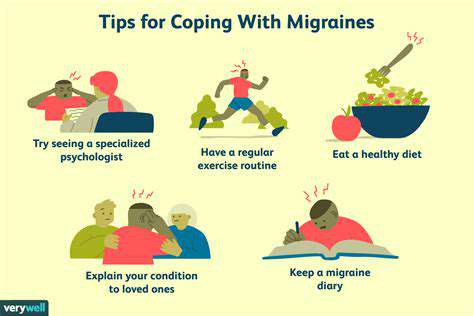
Management Strategies for Migraine Allodynia
Managing migraine allodynia requires a multifaceted approach targeting both the acute pain and the underlying mechanisms contributing to the heightened sensitivity. This often involves a combination of pharmacological interventions and non-pharmacological strategies. One crucial aspect is meticulous pain management during migraine attacks, utilizing appropriate medications as prescribed by the physician to alleviate the acute pain and associated allodynia. This might include triptans, or other migraine-specific medications, combined with pain relievers to effectively control the episode.
Alongside pharmacological treatments, non-pharmacological approaches play a vital role in managing migraine allodynia. These include lifestyle modifications, such as stress reduction techniques, regular sleep patterns, and a balanced diet. Cognitive behavioral therapy (CBT) can be valuable in helping patients cope with the emotional and psychological impact of chronic pain and allodynia. Physical therapy, including specific exercises and manual therapies, can also help improve function and reduce pain perception. Furthermore, identifying and avoiding specific triggers, like certain foods, smells, or environmental factors, can be instrumental in minimizing the frequency and severity of attacks.
Impact of Allodynia on Daily Life
Migraine allodynia significantly impacts the daily lives of those affected. The heightened sensitivity to touch, sound, light, or other stimuli can drastically limit participation in daily activities, impacting work, school, social interactions, and even simple household tasks. The constant pain and discomfort can lead to feelings of isolation, frustration, and decreased quality of life. This can manifest in difficulty concentrating, reduced productivity, and a general sense of fatigue. Furthermore, the emotional distress associated with chronic pain can contribute to anxiety, depression, and other mental health challenges.
The persistent nature of migraine allodynia necessitates the development of coping mechanisms and support systems. Understanding the impact of the condition on daily life is crucial for developing effective management strategies and ensuring that patients receive the necessary support to maintain their well-being and quality of life. This understanding also empowers patients to advocate for their needs and work collaboratively with healthcare professionals to develop personalized treatment plans. This often includes support from family, friends, and support groups.
Living with Migraine Allodynia: Coping Strategies
Understanding Migraine Allodynia
Migraine allodynia is a debilitating condition where individuals experience heightened sensitivity to normally harmless stimuli. This heightened sensitivity can manifest in various ways, from the touch of a light breeze becoming excruciating to the sound of a ticking clock causing unbearable pain. This sensitivity extends beyond the typical migraine pain zone, affecting areas that would normally not cause discomfort. This can make daily tasks and activities incredibly challenging and significantly impact quality of life.
It's crucial to understand that migraine allodynia is not simply a more intense form of migraine. It's a distinct feature of the condition, often characterized by a profound shift in the body's perception of sensory input. The underlying mechanisms are still being researched, but it's believed to involve changes in the central nervous system's processing of pain signals.
Managing Sensory Overload
Managing the sensory overload associated with migraine allodynia requires a multifaceted approach. Identifying triggers, like specific sounds, smells, or textures, is paramount. Once identified, individuals can actively work to minimize exposure to these triggers. This might involve using noise-canceling headphones, wearing sunglasses, or even altering their daily routines to avoid triggering situations.
Effective pain management strategies are also essential. These might include over-the-counter pain relievers, prescription medications, or alternative therapies such as acupuncture or biofeedback. Finding the right combination of treatments can significantly reduce the intensity and frequency of attacks. It's often a process of trial and error to discover what works best for each individual.
Relaxation techniques, such as deep breathing exercises and mindfulness meditation, can also help to manage stress and anxiety, which can often exacerbate migraine allodynia symptoms.
Lifestyle Adjustments and Support Systems
Lifestyle adjustments play a vital role in managing migraine allodynia. A consistent sleep schedule, a balanced diet, and regular exercise can help to regulate the body's natural rhythms and potentially reduce the likelihood of attacks. Furthermore, maintaining a healthy weight and staying hydrated are important aspects of overall well-being.
A strong support system is crucial for individuals living with migraine allodynia. Sharing experiences and seeking advice from others who understand the condition can provide invaluable emotional support and practical guidance. Connecting with support groups or online communities dedicated to migraine sufferers can offer a sense of belonging and a platform for shared experiences. Talking to healthcare professionals is equally important, as they can provide personalized guidance and management strategies tailored to individual needs.
It's important to remember that managing migraine allodynia is an ongoing process. Patience, persistence, and open communication with healthcare providers are key to finding the most effective strategies for pain relief and improved quality of life.