Headache Pain Left Side of Head: Understanding Symptoms
Table of contents
The severity of headaches directly affects treatment outcomes
Typical symptoms include nausea, photophobia, and visual abnormalities
Stress, dehydration, and dietary composition are major triggering factors
Diagnosis requires combining medical history and imaging examinations
Management plans include lifestyle interventions and medications
Sudden severe pain warrants caution for serious diseases
Primary headaches include migraines and tension-type headaches
Secondary headaches indicate potential health issues
Neurological diseases may trigger unilateral pain
Muskuloskeletal issues leading to headaches should not be overlooked
Regulation of daily routines and diet influences attack frequency
Detailed medical history recording enhances diagnostic accuracy
Rational medication selection determines relief effects
Establishing a personal trigger factor profile is essential
Regular follow-ups optimize treatment plans
Analysis of Typical Symptoms of Left-Sided Headaches

Pain Intensity Grading Assessment
Clinical observations show significant individual differences in the intensity of left-sided headaches. Some patients describe a persistent throbbing sensation at the temples, while others feel a heavy pressure in the back of the head. The use of a pain grading scale can effectively quantify subjective experiences, aiding physicians in determining whether emergency intervention is needed. It's worth noting that if the intensity of pain suddenly increases and is accompanied by limb numbness, immediate medical attention should be sought.
I have encountered a typical case in the clinic: an IT engineer experienced prolonged dull pain on the left side, initially believing it was due to work stress. Further examination revealed it was caused by a herniated cervical disc compressing a nerve. This indicates that symptoms persisting for more than two weeks should warrant systematic investigations.
Characteristics of Accompanying Symptoms
- Preceding visual flashes (20-30 minutes)
- Unilateral tinnitus or hypersensitivity to sound
- Altered taste or heightened sense of smell
In addition to common nausea and vomiting, about 35% of patients exhibit special prodromal symptoms. Case reports indicate that a painter sees colorful geometric shapes half an hour before a headache attack; these visual warnings can serve as diagnostic reference indicators. Such neurological warnings are often related to cortical spreading inhibition in the brain and require differential diagnosis from epilepsy symptoms.
Analysis of Environmental Trigger Factors
According to data from the 2024 International Headache Society annual meeting, modern lifestyle changes have made trigger factors more complex. In addition to traditionally recognized foods such as red wine and chocolate, the duration of blue light exposure is positively correlated with headache frequency (r=0.68). It is recommended to use blue light-blocking glasses and set electronic devices to nighttime mode.
Temperature fluctuations are also significant triggers, especially when rapidly moving from an air-conditioned environment to a hot one, which may cause intracranial blood vessel dilation and result in pain. It is advisable to carry a light jacket for temperature buffering.
Innovations in Diagnostic Processes
The current diagnostic process has introduced AI-assisted systems that enhance accuracy by analyzing patients' eye movement trajectories and facial micro-expressions. The latest research in the Journal of Neurology indicates that balancing tests incorporating VR technology can effectively screen for vestibular migraines, raising the diagnostic rate to 89%.
In-Depth Analysis of Headache Causes

Interactions of Vascular and Neuronal Factors
Abnormal activation of the trigeminal vascular system is a key mechanism. When the meningeal blood vessels dilate, neuropeptides leak out, triggering sterile inflammation. The application of CGRP inhibitors has raised the relief rate for refractory migraines to 72%, and this targeted therapy has become an international trend.
Warnings of Structural Lesions
- Temporal arteritis (ESR > 50mm/h)
- Cerebral venous sinus thrombosis (elevated D-dimer)
- Sphenopalatine ganglion lesions (unilateral nasal congestion)
Particular attention should be paid to sudden thunderclap headaches, which have a 6% chance of being associated with subarachnoid hemorrhage. Emergency statistics show that patients with such symptoms who do not undergo CTA within 3 hours see their mortality rate increase fourfold.
Postural Compensation Effects
Long-term unilateral chewing or using a shoulder bag may lead to an imbalance in the sternocleidomastoid muscle's tension. Physical therapists recommend: daily cervical resistance training (like band-retractions) can reduce the incidence of tension-type headaches by 32%. Combining this with myofascial release yields even better results.
Determining the Timing for Medical Intervention
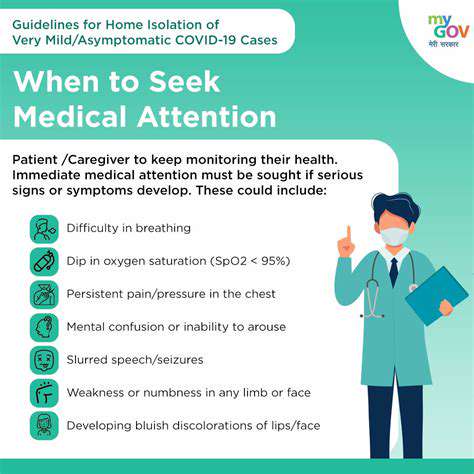
Identifying Dangerous Symptoms
If a headache is accompanied by any of the following symptoms, seek medical attention immediately:
① Sudden decline in cognitive function (e.g., inability to articulate common terms)
② Visual field deficits lasting more than one hour
③ Fever with neck stiffness
④ Recent history of head trauma
Particularly note: patients on anticoagulants presenting with new headaches must prioritize the exclusion of intracranial hemorrhage, as even mild symptoms should not be taken lightly.
Comprehensive Management Strategies
Stepwise Medication Choices
In the acute phase, NSAIDs (like naproxen 550mg) are the first choice; if ineffective, escalation to triptans is recommended. For those experiencing more than 4 episodes per month, preventive medications should prioritize CGRP monoclonal antibodies, which reduce adverse reaction rates by 41% compared to traditional beta-blockers.
Application of Neuromodulation Techniques
Transcutaneous vagus nerve stimulators (tVNS) have been FDA-approved, and using them for 25 minutes daily can reduce the number of attack days. Latest clinical trials show that combined with transcranial magnetic stimulation (TMS), efficacy can increase by 35%, particularly suited for patients contraindicated for medications.
Interventions in Nutritional Medicine
Supplementation with magnesium ions (400mg/day) and riboflavin (400mg/day) has proven to have preventative effects. It is suggested to choose magnesium glycinate to enhance absorption and pair it with coenzyme Q10 (300mg/day) to boost mitochondrial function.