Problem Solving
Root Cause Analysis
Headache Location
Sinus Pain
HTML element
CSS class
Headaches
Sinus Infections
HTML
Styling
صداع الجيوب الأنفية أم الصداع النصفي؟ كيفية التمييز بينهما؟
اختلافات رئيسية

فهم السبب الجذري
تحديد المصدر الدقيق للألم أمر بالغ الأهمية لإدارة فعالة.
أعراض صداع الجيوب الأنفية: الموقع والخصائص
موقع صداع الجيوب الأنفية: المناطق الرئيسية
غالباً ما يظهر صداع الجيوب الأنفية في مناطق محددة من الرأس، مما يعكس موقع الجيوب الأنفية الملتهبة. عادةً ما يكون الألم مركزاً حول
أسباب والمحفزات المرتبطة: الكشف عن الأسباب
فهم آلام الجيوب الأنفية
غالباً ما تُصنف آلام الجيوب الأنفية، التي تتميز عادةً بألم موضعي في الجبهة، أو الخدين، أو حول العينين، على أنها صداع نصفي، مما يؤدي إلى خطأ في التشخيص. عدم
Read more about صداع الجيوب الأنفية أم الصداع النصفي؟ كيفية التمييز بينهما؟
الأعراض والأسباب والعلاج
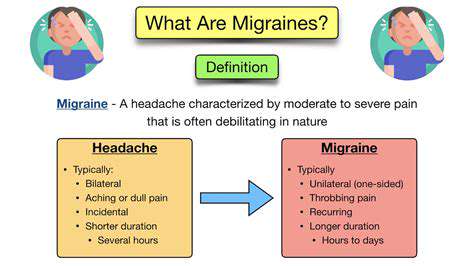
فهم الصداع في الجانب الأيسر أمر بالغ الأهمية للإدارة والعلاج الفعال. يستعرض هذا الدليل المعلوماتي طبيعة الصداع في الجانب الأيسر، والأعراض الشائعة، والأسباب المحتملة، والإجراءات الموصى بها عند البحث عن التخفيف.
فهم صداع الجانب الأيسر
يمكن أن تختلف آلام الصداع في الجانب الأيسر بشكل كبير من حيث الشدة والجودة، وغالبًا ما يصف الأفراد الألم بأنه نابض أو ضغط مستمر. هذه الفروقات حيوية للمهنيين الصحيين لتطوير استراتيجيات علاج مناسبة. وقد أظهرت الأبحاث أن الصداع الموجود في الجانب الأيسر قد يرتبط بمختلف الحالات مثل الصداع النصفي ويتأثر بعوامل نمط الحياة مثل التوتر واضطرابات النوم.
الأعراض الشائعة
تشمل الأعراض التي ترافق عادةً الصداع في الجانب الأيسر حساسية للضوء أو الصوت، والغثيان، واضطرابات بصرية. يمكن أن يساعد الاحتفاظ بمذكرة للصداع تتبع بداية الألم والمدة والأعراض المرتبطة في تحديد المحفزات الخاصة وإبلاغ طرق العلاج.
الأسباب المحتملة
1. الصداع الأولي: هذه الأنواع من الصداع المستقل تشمل الصداع النصفي، والصداع التوتري، وصداع المجموعات. يُعرف الصداع النصفي بأنه ألم أحادي الجانب وقد يتضمن أعراضًا إضافية مثل الغثيان والحساسية للضوء. وغالبًا ما تنشأ الصداع التوتري من التوتر أو وضعية غير صحيحة، وغالبًا لا تتضمن الغثيان.
2. الصداع الثانوي: هذه الأعراض تكون دالة على حالات كامنة، مثل التهاب الجيوب الأنفية، مما قد يؤدي إلى الألم المرتبط بالجانب الأيسر من الرأس. نادراً ما يمكن أن تظهر حالات أكثر خطورة مثل السكتة الدماغية على شكل صداع موضعي.
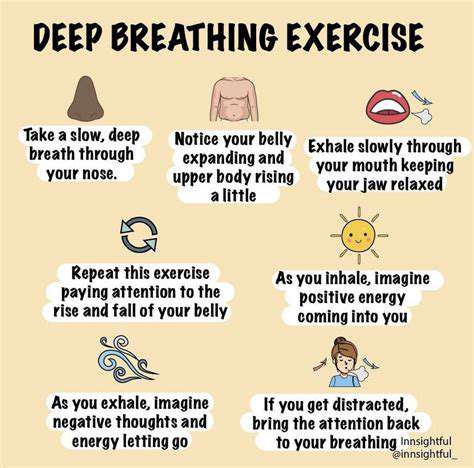
3. عوامل نمط الحياة: يمكن أن تلعب الضغوط العاطفية والمشكلات العضلية الهيكلية واستخدام الأدوية بشكل مفرط دور المحفزات. يمكن أن يساعد الحفاظ على وضعية جيدة وتقليل التوتر من خلال تقنيات الاسترخاء في تخفيف تكرار الصداع.
متى يجب طلب المساعدة
من الضروري التعرف على متى يجب عليك طلب الرعاية الطبية. يجب تقييم الصداع الحاد الذي يحدث فجأة، أو الأعراض العصبية أو الألم المستمر بشكل احترافي على الفور. علاوة على ذلك، إذا فشلت الأدوية التي لا تتطلب وصفة طبية في توفير التخفيف، يمكن أن يؤدي استشارة متخصص في الرعاية الصحية إلى خطة علاج أكثر تخصيصًا.
استراتيجيات التخفيف الفعالة
الإجراءات الوقائية
يمكن أن يؤدي تنفيذ نمط حياة متوازن - ممارسة الرياضة بانتظام، والنظام الغذائي المناسب، والترطيب الجيد، وإدارة التوتر بشكل فعال - إلى تقليل تكرار وشدة الصداع في الجانب الأيسر بشكل كبير.
خيارات العلاج
تعمل الأدوية التي لا تتطلب وصفة طبية مثل الإيبوبروفين أو الاسيتامينوفين كخط دفاع أول، ولكن يجب توخي الحذر لتجنب الصداع الارتدادي الناتج عن الاستخدام المفرط. يمكن أن تقدم العلاجات البديلة، بما في ذلك الوخز بالإبر وممارسات اليقظة، فوائد كبيرة أيضًا.
الختام
يعتبر فهم الصداع في الجانب الأيسر أمرًا محوريًا لتحقيق تخفيف وإدارة فعالة. من خلال التعرف على الأعراض، وتحديد المحفزات المحتملة، ومعرفة متى تطلب النصيحة الطبية، يمكن للأفراد تحسين جودة حياتهم بشكل كبير. سواء كان ذلك من خلال تغييرات في نمط الحياة أو علاجات احترافية، يمكن أن يؤدي التعامل مع هذه الصداع إلى حياة أكثر صحة ورضا.
لمزيد من الإرشادات التفصيلية، تعمق في المواضيع مثل [كيفية تحديد المحفزات للصداع]() أو تعلم المزيد حول [متى تطلب الرعاية الطبية]().
Apr 18, 2025
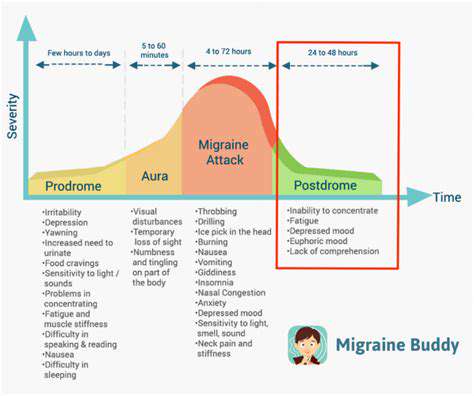
الفهم والتخفيفمتلازمة ما بعد الصداع النصفي، التي تُعرف غالبًا باسم الصداع النصفي الكحول، هي مرحلة تلي الصداع الشديد و أعراض نوبة الصداع النصفي. خلال هذه الفترة من التعافي، قد يختبر الأفراد
May 06, 2025
المغنيسيوم والصداع النصفي: هل المكملات الغذائية تساعد؟
May 13, 2025
دور العلاج الطبيعي في إدارة بعض أنواع الصداع
May 18, 2025
استخدام الهرمونات البيولوجية المماثلة لصداع التوتر الهرموني: إيجابيات وسلبيات
May 22, 2025
استخدام العلاج بالموسيقى للاسترخاء وإدارة الألم
May 29, 2025
فهم الصداع الناجم عن الإفراط في استخدام الأدوية (صداع الارتداد)
Jun 06, 2025
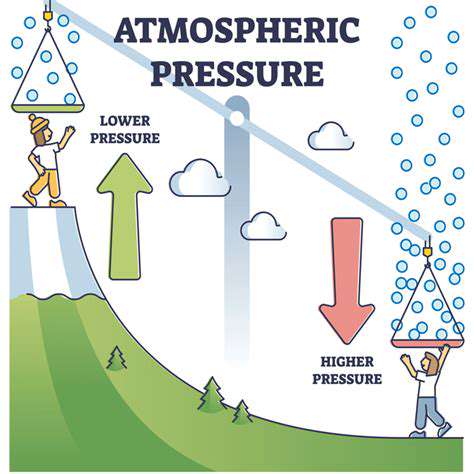
ما الذي يُسبب الصداع النصفي حقًا؟ استكشاف العلم
Jun 10, 2025
هل يمكن لتطبيقات الطقس التنبؤ بأيام خطر الإصابة بالصداع النصفي؟
Jun 30, 2025
صداع النصفي مقابل الصداع: فهم الاختلافات الرئيسية
Jul 02, 2025
التخطيط المسبق: استراتيجيات للوقاية من الصداع النصفي
Jul 07, 2025
إنشاء خطة عمل لليوم الذي يهاجم فيه الصداع النصفي
Jul 07, 2025