Sinus Headache or Migraine? How to Tell the Difference

Understanding the Root Cause
Pinpointing the exact source of the pain is crucial for effective management. This involves a thorough examination of the situation, considering all contributing factors, and not just focusing on the immediate symptom. Identifying the root cause allows for targeted interventions that address the underlying issue rather than merely treating the surface manifestation. A holistic approach is essential to achieve long-term solutions and prevent future recurrences.
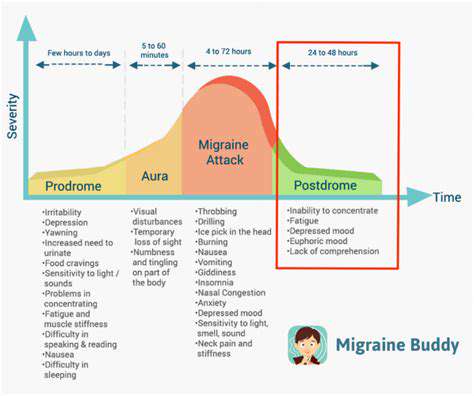
Recognizing the Symptoms
Careful observation of the symptoms is vital. This includes noting the specific characteristics of the pain, such as its location, intensity, duration, and frequency. Are there any other accompanying symptoms, like swelling, redness, or fever? Detailed documentation of these symptoms will provide valuable information for diagnosis and treatment planning. Furthermore, understanding the context of the pain, such as when it occurs or what triggers it, can significantly aid in identifying patterns and potential causes.
Assessing the Impact
Evaluating the impact of the pain on daily life is essential. How does it affect your ability to work, sleep, and participate in social activities? Assessing the functional limitations imposed by the pain is crucial for prioritizing treatment strategies. The impact on overall well-being should be considered, including its effects on emotional and mental health.
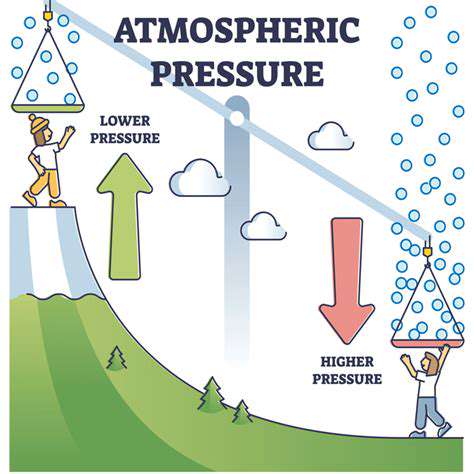
Considering External Factors
External factors, both physical and environmental, can significantly contribute to pain. Environmental stressors such as excessive noise, poor ergonomics, or repetitive movements can be major contributors. Identifying these factors is important for developing preventative measures and strategies to mitigate their impact. Chronic pain can also be exacerbated by psychological factors like stress and anxiety. Understanding these elements is vital for a comprehensive approach.
Exploring Potential Medical Conditions
A thorough examination is necessary to rule out any underlying medical conditions. Consult with a healthcare professional to discuss any potential medical conditions that might be contributing to the pain. This includes reviewing medical history, conducting physical examinations, and potentially ordering diagnostic tests. This step is crucial to ensure that any serious underlying medical issues are addressed promptly.
Lifestyle Modifications
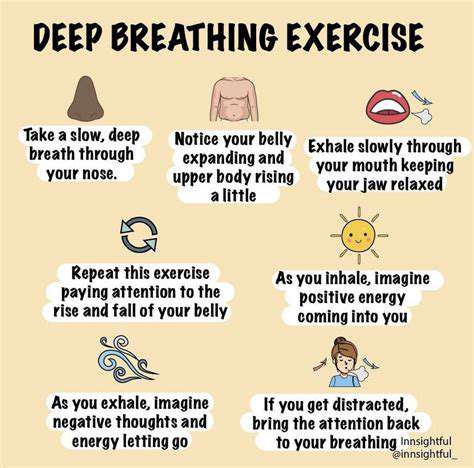
Lifestyle changes can play a significant role in managing pain. This includes adopting healthier habits such as regular exercise, maintaining a balanced diet, and getting sufficient rest. These adjustments can positively impact overall health and well-being, reducing the likelihood of pain flare-ups. Furthermore, stress management techniques, such as meditation or yoga, can be beneficial in alleviating pain related to stress or anxiety.
Seeking Professional Guidance
Seeking professional guidance is paramount in managing persistent pain. Consulting with healthcare professionals, such as doctors, physical therapists, or pain management specialists, is critical for developing an effective treatment plan. These professionals can provide expert guidance and support to address the specific needs of the individual. Their expertise ensures that the treatment approach is tailored to the individual's unique circumstances and medical history.
Sinus Headache Symptoms: Location and Characteristics
Sinus Headache Location: Key Areas
Sinus headaches often manifest in specific areas of the head, reflecting the location of the inflamed sinuses. Commonly, pain is centered around the forehead, the cheeks, or the bridge of the nose. This localized pain can be a key differentiator from other types of headaches, such as migraines, which may present with more diffuse pain across the head.
Pressure and tenderness in these areas are also frequently reported by those experiencing sinus headaches. A person might find they are more sensitive to touch or pressure in the affected region, further distinguishing it from a headache that is more generalized in its pain.
Pain Intensity and Quality
The intensity of sinus headache pain can vary greatly from person to person. Some individuals experience a dull, throbbing ache, while others report a sharp, stabbing pain. Understanding the quality of the pain, whether it's a persistent pressure, a throbbing sensation, or something else, can be helpful in identifying the cause of the headache.
Pain that is worsened by bending over or lying down can also be an indicator of sinus involvement, as the change in posture can affect sinus drainage and pressure.
Associated Symptoms: Beyond the Pain
Sinus headaches are often accompanied by other symptoms. These may include nasal congestion, a runny nose, facial swelling, postnasal drip, and even fever. The presence of these additional symptoms can significantly aid in distinguishing a sinus headache from other types of headaches.
Additionally, some individuals might experience a reduced sense of smell or taste, which can be a helpful symptom to note.
The Role of Sinus Pressure
A key characteristic of a sinus headache is the sensation of pressure within the affected sinus areas. This pressure can feel like a constant ache or a throbbing sensation, often worsening with changes in head position. Recognizing this pressure as a key feature of the headache is essential to accurately diagnosing the issue.
Timing and Duration: When Does It Occur?
Sinus headaches can arise at any time of day, but they often worsen throughout the day, particularly during the day, or in situations that trigger sinus drainage issues. They may be triggered by certain activities, like bending over or lying down, due to the impact on sinus drainage. Understanding the pattern of the headache's onset and duration can be valuable in making a diagnosis.
Factors Influencing Severity
Various factors can influence the severity of a sinus headache. These include allergies, the time of year, and the presence of other infections or illnesses. For example, allergy season often coincides with increased sinus headache frequency and intensity. Tracking these factors can be beneficial for understanding triggers and managing the headaches effectively.
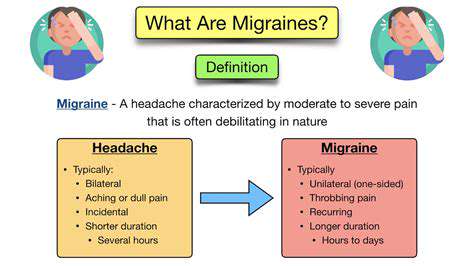
Differentiating from Other Headaches: Important Considerations
It's crucial to distinguish sinus headaches from other types of headaches, such as migraines or tension headaches. While there can be overlaps in symptoms, recognizing the specific characteristics of sinus headaches, including location, pressure, and associated symptoms, can help guide appropriate treatment.
Seeking medical advice is essential for proper diagnosis and management, especially if the headache is severe or accompanied by concerning symptoms.
Triggers and Associated Factors: Unveiling the Causes
Understanding Sinus Headaches
Sinus headaches, often characterized by pain localized to the forehead, cheeks, or around the eyes, are frequently misdiagnosed as migraines. Understanding the specific anatomical location of the sinuses and how inflammation or infection within them can trigger pain is crucial for accurate diagnosis. This localized pain is often accompanied by pressure or fullness in the affected areas, and can be exacerbated by bending over or lying down.
Furthermore, sinus headaches are often associated with other symptoms like nasal congestion, facial tenderness, and a feeling of pressure in the head. Knowing these accompanying symptoms can significantly aid in differentiating sinus headaches from other types of headaches, such as migraines.
Infections and Sinus Inflammation
Infections, particularly viral or bacterial, are common triggers for sinus headaches. The inflammation and swelling caused by these infections can put pressure on the surrounding sinus structures, leading to the characteristic pain. The presence of nasal discharge, often thick and discolored, can further indicate a possible infection as a contributing factor.
Allergies and Environmental Factors
Allergies, whether seasonal or year-round, can significantly impact sinus health. Exposure to allergens can trigger inflammation in the nasal passages and sinuses, leading to swelling and pressure, which can manifest as a sinus headache. In addition, environmental factors such as changes in temperature or humidity can also contribute to sinus inflammation and subsequent headaches.
Furthermore, exposure to irritants like smoke or chemical fumes can trigger similar inflammatory responses, potentially leading to sinus pain and discomfort.
Hormonal Fluctuations and Lifestyle Factors
Hormonal changes, particularly in women, can play a role in the frequency and intensity of sinus headaches. Fluctuations in estrogen levels can affect the lining of the sinuses, making them more susceptible to inflammation. This is often noted during menstruation or pregnancy.
Lifestyle factors like stress, lack of sleep, and poor diet can also contribute to the development of sinus headaches. The body's natural response to stress can exacerbate existing inflammation, potentially leading to more frequent or severe headaches.
Stress and Emotional Factors
While not always a direct cause, stress and emotional factors can significantly influence the experience of sinus headaches. Chronic stress can weaken the immune system, making individuals more susceptible to infections and inflammation, which can trigger sinus pain. Emotional distress can also lead to muscle tension in the head and neck, exacerbating pain perception and increasing the intensity of a headache.
Dietary Sensitivities and Food Intolerances
Certain foods and drinks, while not a direct cause of sinus headaches for everyone, can trigger inflammatory responses in individuals with specific dietary sensitivities or food intolerances. Foods high in histamine, like aged cheeses or fermented foods, can exacerbate symptoms in some people. Keeping a food diary can help identify potential triggers.