Brain Inflammation
Cytokine Signaling
Neurology
Pain Management
Weight Management
Nutritional Strategies
Nutrition
Inflammation
Zapalenie a migrena: zrozumienie związku
Kasada Zapalna w Mózgu
Rola Cytokin w Zapaleniu Mózgu
Cytokiny, zróżnicowana grupa białek sygnalizacyjnych, odgrywają kluczową rolę w koordynacji odpowiedzi zapalnej w mózgu. Te cząsteczki
Czynniki wywołujące stan zapalny i ataki migreny
Rola stanu zapalnego w migrenie
Read more about Zapalenie a migrena: zrozumienie związku
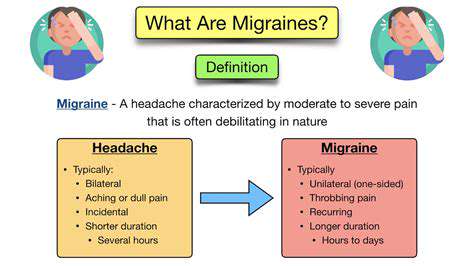
Rodzaje, wyzwalacze i strategie zarządzania Zbadaj różne rodzaje bólu głowy, w tym pierwotne bóle głowy, takie jak migreny i bóle napięciowe, a także wtórne bóle głowy spowodowane innymi stanami medycznymi. Dowiedz się, jak modyfikacje stylu życia, rozważania dietetyczne i czynniki środowiskowe mogą wpływać na częstotliwość i intensywność bólu głowy. Odkryj holistyczne podejścia i skuteczne strategie radzenia sobie w zarządzaniu przewlekłym bólem głowy. Jeśli sama opieka nie jest wystarczająca, dowiedz się, kiedy warto szukać profesjonalnej pomocy w celu uzyskania spersonalizowanych opcji leczenia. Wyposaż się w wiedzę, aby poprawić jakość życia i zmniejszyć ból głowy już dziś!
Oct 10, 2024
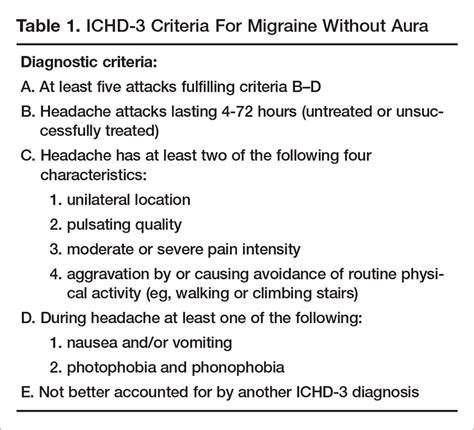
Zrozumienie pulseującego bólu po lewej stronie głowy Zbadaj złożoność pulseującego bólu po lewej stronie głowy, zdobijając wiedzę na temat objawów, powszechnych przyczyn, takich jak bóle głowy napięciowe i migrenowe, oraz skutecznych możliwości leczenia. Ten kompleksowy przewodnik zagłębia się w cechy pulseującego bólu, w tym jego pulsującą naturę i sporadyczność, a także potencjalnie towarzyszące objawy, takie jak nudności i wrażliwość na światło. Dowiedz się, jak czynniki stylu życia, czynniki środowiskowe i stany zdrowotne mogą przyczyniać się do tego dyskomfortu. Poznaj powszechne przyczyny, takie jak migreny, bóle głowy klastrowe oraz zapalenie tętnicy skroniowej, i dowiedz się, kiedy należy szukać pomocy medycznej w przypadku ciężkich objawów. Strona podkreśla również różne strategie zarządzania, w tym możliwości leczenia farmakologicznego, wzięcie pod uwagę diety oraz modyfikacje stylu życia w celu złagodzenia bólu. Wyposaż się w wiedzę, aby skutecznie zarządzać pulseującym bólem i poprawić ogólny dobrostan.
Nov 09, 2024
Zrozumienie Bólu w Lewym Boku Skroni Odkryj złożoności bólu w lewym boku skroni — jego objawy, przyczyny i skuteczne strategie zarządzania. Ten kompleksowy przewodnik obejmuje wszystko, od częstych winowajców, takich jak napięciowe bóle głowy i migreny, po bardziej poważne stany, które mogą wymagać uwagi profesjonalnej. Naucz się rozpoznawać, kiedy należy szukać pomocy medycznej, i eksploruj różnorodne domowe środki, modyfikacje stylu życia i leczenie medyczne w celu łagodzenia dyskomfortu. Pozostawaj świadomy znaczenia rozumienia swoich wzorców bólu głowy i czynników wyzwalających, aby ułatwić dostosowane podejście do leczenia. Umożliw sobie zarządzanie bólem w lewej skroni skutecznie i popraw swoje samopoczucie.
Nov 10, 2024
Opis strony internetowej na temat możliwych przyczyn bólu lewego boku. Odkryj różne potencjalne przyczyny bólu lewego boku, od problemów mięśniowo-szkieletowych po zaburzenia trawienia, problemy sercowo-naczyniowe i czynniki psychologiczne. Ten kompleksowy przewodnik szczegółowo opisuje typowe objawy, potencjalne stanowiące zagrożenie oraz skuteczne opcje leczenia. Zrozum, jak takie czynniki jak zła postawa, problemy związane z nerwami i zdrowie reprodukcyjne mogą przyczyniać się do dyskomfortu. Dowiedz się, jak ważne jest rozpoznawanie konkretnych objawów i jak ważne jest, aby w odpowiednim czasie ubiegać się o pomoc medyczną w przypadku poważniejszych schorzeń. Poznaj opcje leczenia, w tym leki, terapię fizyczną i zmiany stylu życia, aby złagodzić ból i poprawić ogólne samopoczucie. Bądź na bieżąco z informacjami i przejmij kontrolę nad swoim zdrowiem dzięki naszym informacyjnym zasobom.
Nov 20, 2024
Kompleksowy przewodnikZbadaj złożony związek między napięciem mięśniowym a stanem zapalnym w naszym szczegółowym artykule. Odkryj fizjologiczne mechanizmy stojące za napięciem mięśniowym, w tym jak skurcze mięśni mogą prowadzić do dyskomfortu oraz rolę produktów ubocznych metabolizmu. Zgłębiamy znaczenie stanu zapalnego dla zdrowia mięśni, omawiając jego podwójną rolę w procesie gojenia i potencjalne negatywne skutki, gdy staje się przewlekły. Naucz się skutecznych strategii zarządzania napięciem mięśniowym poprzez regularną aktywność fizyczną, rozciąganie i praktyki uważności. Zrozum, jak wybory żywieniowe wpływają zarówno na zdrowie mięśni, jak i stan zapalny, podkreślając korzyści z diety przeciwzapalnej bogatej w niezbędne witaminy i minerały. Ten przewodnik porusza również powszechne przyczyny napięcia mięśniowego, od stresu i złej postawy po nawadnianie i odżywianie, wyposażając cię w wiedzę do proaktywnego zarządzania zdrowiem. Dzięki spostrzeżeniom na temat skutecznych technik łagodzenia bólu, w tym terapiach profesjonalnych i domowych środkach zaradczych, możesz poprawić swoje zdrowie mięśni i ogólne samopoczucie. Słowa kluczowe: napięcie mięśniowe, stan zapalny, zdrowie mięśni, dieta przeciwzapalna, zarządzanie stresem, ćwiczenia, regeneracja.
Nov 20, 2024
Magnez i migrena: Czy suplementacja pomaga?
May 13, 2025
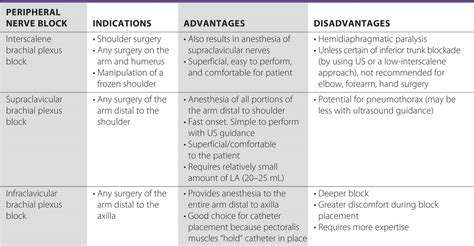
Blokady nerwowe w leczeniu bólu głowy: Co musisz wiedzieć
May 24, 2025
Zrozumienie bólu głowy pochodzenia szyjnego: Kiedy ból szyi powoduje ból głowy
Jun 04, 2025
Badanie adaptogenów w leczeniu migren związanych ze stresem
Jun 26, 2025
Badanie igłoleczenia suchego w przypadku bólu mięśniowo-powięziowego i bólu głowy
Jul 02, 2025
Co się dzieje podczas wizyty u neurologa z powodu migreny?
Jul 21, 2025
Rozumienie nerwobólu potylicznego: Przyczyna bólu głowy
Jul 22, 2025