Inflammation and Migraines: Understanding the Connection
The Inflammatory Cascade in the Brain
The Role of Cytokines in Brain Inflammation
Cytokines, a diverse group of signaling proteins, play a pivotal role in orchestrating the inflammatory response within the brain. These molecules, produced by various cells within the central nervous system, act as messengers, triggering a cascade of events that can lead to increased blood flow, swelling, and pain perception. Understanding the specific types and levels of cytokines involved in migraine pathogenesis is crucial for developing targeted therapeutic strategies.
Different cytokines, such as TNF-α and IL-1β, exhibit pro-inflammatory properties, contributing to the activation of immune cells and the release of further inflammatory mediators. This intricate network of interactions significantly influences the overall inflammatory state of the brain, which can potentially contribute to the development and severity of migraine episodes.
Neurovascular Coupling and Inflammation
The intricate relationship between the nervous system and the circulatory system, known as neurovascular coupling, is significantly impacted by inflammation. During a migraine attack, this coupling can become disrupted, leading to alterations in cerebral blood flow. This disruption is often associated with the release of inflammatory mediators, further exacerbating the neurovascular imbalance.
The resulting changes in blood vessel dilation and constriction contribute to the characteristic throbbing pain and other symptoms associated with migraines. Understanding the precise mechanisms through which inflammation disrupts neurovascular coupling is vital for developing strategies to restore normal function and reduce migraine pain.
The Role of Astrocytes and Microglia
Astrocytes and microglia, specialized glial cells within the brain, are key players in the inflammatory cascade. Astrocytes, responsible for maintaining the integrity of the extracellular environment, can become activated during inflammatory responses, releasing various inflammatory mediators that contribute to the overall inflammatory process.
Microglia, the brain's resident immune cells, are activated in response to various stimuli, including migraine triggers. Their activation leads to the release of pro-inflammatory cytokines and other mediators that amplify the inflammatory response, potentially contributing to the perpetuation of migraine pain.
The Impact of Genetic Predisposition
Genetic factors play a significant role in determining an individual's susceptibility to migraine. Variations in genes encoding proteins involved in the inflammatory cascade, neurotransmission, and neurovascular coupling can influence the individual's response to migraine triggers and the intensity of the resulting inflammatory response.
Studies have identified specific genetic markers associated with a higher risk of migraine development. Further research focusing on these genetic predispositions could lead to more precise diagnostic tools and personalized treatment approaches for migraine sufferers.
The Link Between Inflammation and Pain Perception
Inflammation within the brain can significantly alter pain perception pathways, making individuals more sensitive to pain during a migraine attack. The release of inflammatory mediators can sensitize nociceptive neurons, leading to an amplified response to noxious stimuli. This heightened sensitivity to pain can contribute to the throbbing and pulsating nature of migraine pain.
The Role of Environmental Factors
Environmental factors, such as stress, sleep deprivation, and dietary triggers, can influence the inflammatory response within the brain, potentially contributing to migraine development. Chronic stress, for example, can activate the hypothalamic-pituitary-adrenal (HPA) axis, leading to the release of stress hormones that can trigger an inflammatory cascade in the brain.
Understanding the interplay between environmental factors and the inflammatory cascade is critical for developing preventive strategies and lifestyle modifications to mitigate the risk and severity of migraine attacks.
Therapeutic Targets for Migraine Management
Targeting the inflammatory cascade offers a promising avenue for developing novel migraine treatments. By focusing on specific inflammatory mediators or pathways, researchers hope to develop medications that effectively reduce or prevent the inflammatory response within the brain during a migraine attack.
These strategies could potentially alleviate the pain, reduce the frequency, and minimize the severity of migraine episodes. Exploring the development of anti-inflammatory agents specifically designed to target the brain's inflammatory response is a key area of ongoing research.
Inflammation Triggers and Migraine Attacks
Inflammation's Role in Migraine
Inflammation plays a crucial role in the development and progression of migraine attacks. While the exact mechanisms are still under investigation, research strongly suggests that inflammatory processes within the brain and surrounding tissues contribute significantly to the pain, sensitivity, and other symptoms associated with migraine. Understanding the specific inflammatory pathways involved is key to developing more effective treatments. Inflammation is a complex process involving various cells and molecules, and its dysregulation can lead to a cascade of events that trigger migraine.
Inflammation is not merely a consequence of a migraine attack; it appears to be an active participant in the attack itself. This suggests that targeting inflammatory responses could be a promising avenue for preventative and therapeutic strategies. Further research into the specific inflammatory mediators and their interplay with migraine triggers is necessary to fully elucidate the relationship.
Genetic Predisposition to Inflammation
Genetic factors are known to influence an individual's susceptibility to various inflammatory conditions, including migraine. Individuals with a family history of migraine are more likely to develop the condition themselves, and this increased risk is often linked to genetic variations that affect the body's inflammatory response. Specific genes that code for proteins involved in inflammation are potential targets for future research into migraine prevention and treatment.
These genetic predispositions may influence the way the body responds to various triggers, making some individuals more vulnerable to migraine attacks. Further research is needed to pinpoint the exact genes and their impact on inflammatory pathways associated with migraine.
Dietary Factors and Inflammation
Certain dietary choices can have a significant impact on inflammation levels in the body. Foods high in processed sugars, saturated fats, and unhealthy trans fats are often associated with increased inflammation. A diet rich in fruits, vegetables, and whole grains, on the other hand, has been shown to have anti-inflammatory properties, potentially mitigating migraine risk.
The interplay between diet, inflammation, and migraine is a complex area of research, and further studies are needed to establish definitive links and personalized dietary recommendations. Maintaining a balanced and nutritious diet is crucial for overall health, including managing migraine risk factors.
Stress and the Inflammatory Response
Chronic stress is a significant environmental factor that can trigger or exacerbate inflammatory responses in the body. The stress response system releases hormones that can directly impact the immune system, leading to increased inflammation. Stress-related inflammation may contribute to the development and intensity of migraine headaches.
Stress management techniques, such as mindfulness, yoga, and meditation, may help regulate the inflammatory response and reduce the frequency and severity of migraine attacks. Addressing stress as a potential trigger is crucial for developing comprehensive migraine management strategies.
Environmental Triggers and Inflammation
Environmental factors, such as exposure to allergens, pollutants, and changes in barometric pressure, can also trigger or worsen inflammatory responses in the body. These triggers can directly or indirectly impact the nervous system, leading to migraine pain and other symptoms. Furthermore, environmental stressors can exacerbate pre-existing inflammatory conditions, further increasing the likelihood of migraine attacks.
Identifying specific environmental triggers and developing effective strategies to mitigate their effects is an important aspect of migraine management. This may involve lifestyle modifications, environmental controls, and potentially targeted therapies to modulate the inflammatory response to environmental factors.
Sleep Deprivation and Inflammation
Sleep deprivation is a significant lifestyle factor that can significantly increase inflammation in the body. A lack of sufficient sleep disrupts the body's natural regulatory mechanisms, leading to an imbalance in various inflammatory pathways. Poor sleep quality and insufficient sleep duration are often cited by migraine sufferers as triggers.
Prioritizing adequate sleep hygiene, establishing a regular sleep schedule, and creating a conducive sleep environment can help to mitigate the inflammatory response associated with sleep deprivation and reduce the risk of migraine attacks. This underlines the importance of sleep as a crucial component in overall health and migraine management.
Inflammation Markers and Migraine Diagnosis
Understanding the Role of Inflammation in Migraines
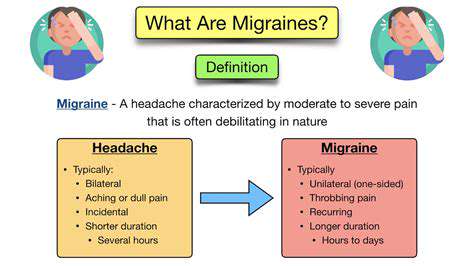
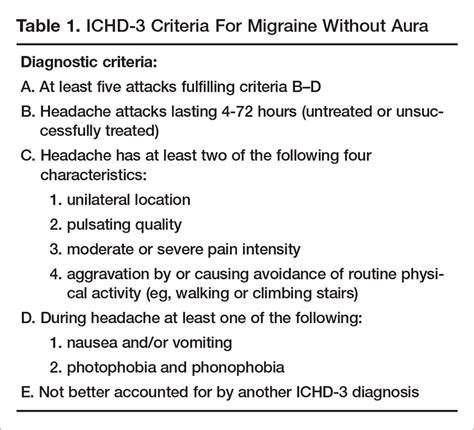
Inflammation plays a crucial role in the pathophysiology of migraines, a debilitating neurological disorder characterized by severe headaches. While the exact mechanisms are still under investigation, mounting evidence suggests that inflammatory processes contribute significantly to the pain, sensory disturbances, and other symptoms associated with migraine attacks. Understanding these inflammatory pathways is vital for developing more effective diagnostic and therapeutic strategies.
Inflammation, typically a protective response to injury or infection, involves the activation of immune cells and the release of inflammatory mediators. In migraine, these processes appear to be dysregulated, leading to an excessive and prolonged inflammatory response within the brain and surrounding tissues. This heightened inflammatory state may contribute to the characteristic throbbing pain, nausea, and sensitivity to light and sound experienced by migraine sufferers.
Inflammation Markers as Potential Diagnostic Tools
Several biological markers, reflecting various aspects of the inflammatory response, have shown promise as potential diagnostic tools for migraines. These markers, often present in the blood or cerebrospinal fluid, can potentially help differentiate migraine from other headache types and identify individuals at higher risk for migraine attacks. The identification of specific inflammation markers could revolutionize diagnostic approaches, enabling earlier and more accurate diagnoses, which is crucial for prompt treatment and management.
Researchers are actively investigating a range of inflammatory markers, including cytokines, chemokines, and proteins involved in the inflammatory cascade. Analyzing these markers in patient samples could provide valuable insights into the underlying inflammatory processes and potentially identify individuals prone to migraine attacks, allowing for proactive interventions.
Current Research on Inflammation Markers and Migraine
Recent studies have explored the correlation between specific inflammatory markers and migraine characteristics, such as attack frequency, severity, and associated symptoms. These investigations have yielded promising results, highlighting the potential of certain markers to predict migraine attacks and potentially personalize treatment approaches. However, more research is still needed to establish robust diagnostic criteria based on these markers.
Ongoing research efforts are focused on identifying the most reliable and sensitive inflammatory markers for migraine diagnosis. Further investigation into the precise mechanisms by which these markers contribute to the migraine experience is also critical. This deeper understanding will pave the way for the development of targeted therapies that specifically address the inflammatory processes underlying migraine attacks.
Potential Limitations and Future Directions
While promising, the use of inflammation markers in migraine diagnosis faces certain limitations. The variability in marker levels among individuals and the influence of other factors, such as stress and diet, need to be considered. Standardization of testing procedures and further validation of these markers across diverse populations are crucial for ensuring reliable and accurate results. Further research is essential to refine diagnostic approaches and develop more effective and targeted treatment strategies.
Future research should focus on developing more sophisticated diagnostic algorithms that integrate inflammatory markers with other clinical data, such as headache characteristics and patient history. The ultimate goal is to create a comprehensive diagnostic tool that can accurately identify migraineurs and tailor treatment plans to individual needs. This will significantly improve the quality of life for millions affected by this debilitating neurological disorder.
Dietary Interventions for Managing Inflammation and Migraine

Nutritional Strategies for Weight Management
Dietary interventions play a crucial role in managing weight, and a personalized approach is key to success. Understanding caloric intake and expenditure is fundamental to any weight management plan. This requires careful consideration of portion sizes, choosing nutrient-dense foods, and incorporating regular physical activity. A balanced diet rich in fruits, vegetables, lean proteins, and whole grains is essential for sustained weight loss or maintenance.
Focusing on nutrient-dense foods can significantly impact weight management. These foods are packed with vitamins, minerals, and fiber, promoting satiety and preventing nutrient deficiencies. Limiting processed foods, sugary drinks, and excessive amounts of unhealthy fats is equally important in achieving sustainable weight goals. Implementing gradual changes in dietary habits, rather than drastic measures, is often more effective for long-term success.
Dietary Approaches for Chronic Disease Prevention
Certain dietary patterns are strongly associated with a reduced risk of chronic diseases such as heart disease, type 2 diabetes, and some cancers. A diet rich in fruits, vegetables, and whole grains can significantly lower the risk of these conditions. These foods provide essential vitamins, minerals, and fiber, promoting overall health and well-being.
The Mediterranean diet, characterized by its emphasis on olive oil, fruits, vegetables, whole grains, and fish, is often cited as a valuable approach. It has been linked to a lower risk of cardiovascular diseases. Similarly, a plant-based diet, emphasizing fruits, vegetables, legumes, and whole grains, has shown promising results in reducing the risk of chronic diseases. Consult a registered dietitian or healthcare professional for personalized dietary recommendations based on individual needs and health conditions.
Dietary Modifications for Specific Health Conditions
Individuals with specific health conditions, such as diabetes, high blood pressure, or digestive disorders, may require specific dietary modifications. A registered dietitian can provide personalized guidance tailored to individual needs and health conditions. Dietary modifications can help manage symptoms and prevent complications. For example, individuals with diabetes may need to carefully monitor their carbohydrate intake, while those with high blood pressure may need to reduce their sodium intake.
Dietary interventions are often a crucial component of managing specific health conditions. For conditions such as celiac disease or inflammatory bowel disease, dietary restrictions are often necessary to alleviate symptoms and prevent further complications. Following a prescribed diet under the supervision of a healthcare professional is crucial in such cases.
The Role of Food in Mental Well-being
Emerging research suggests a strong link between diet and mental well-being. Certain nutrients, such as omega-3 fatty acids, vitamin D, and B vitamins, may play a significant role in maintaining mental health. A balanced diet rich in these nutrients is associated with a reduced risk of depression and anxiety. Moreover, proper nutrition can enhance cognitive function and overall mood.
Sustainable Dietary Practices for Long-Term Health
Adopting sustainable dietary practices is essential for long-term health and well-being. This involves making gradual, manageable changes to eating habits that can be maintained over time. Prioritizing whole, unprocessed foods and limiting highly processed, sugary, and fatty foods is crucial. This includes focusing on nutrient-dense foods such as fruits, vegetables, lean proteins, and whole grains. Educating oneself about healthy eating habits and seeking professional guidance for personalized plans is also important for long-term success.
Lifestyle Factors and the Impact on Inflammation
Dietary Influences on Inflammation
Diet plays a crucial role in regulating inflammation throughout the body. A diet rich in processed foods, saturated fats, and refined sugars can contribute to chronic inflammation, potentially exacerbating migraine symptoms. These foods often lack essential nutrients and antioxidants that are vital for maintaining a healthy inflammatory response. Conversely, a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce inflammation and potentially lessen the frequency and intensity of migraines. A diet high in omega-3 fatty acids, found in fatty fish like salmon and flaxseed, is particularly beneficial in modulating inflammatory processes.
Furthermore, specific dietary components like excessive caffeine or alcohol can trigger or worsen migraine attacks in some individuals. Understanding your individual dietary triggers is crucial for managing inflammation and migraines effectively. Keeping a detailed food journal, noting the types and amounts of food consumed alongside migraine episodes, can help identify patterns and make informed dietary choices to minimize inflammation-related migraines.
Stress Management and Inflammatory Responses
Chronic stress is a significant contributor to inflammation in the body. The body's response to stress activates the hypothalamic-pituitary-adrenal (HPA) axis, which can lead to the release of stress hormones like cortisol. Elevated cortisol levels are associated with increased inflammation, potentially increasing the likelihood and severity of migraine attacks.
Effective stress management techniques, such as regular exercise, mindfulness practices like meditation and deep breathing, and sufficient sleep, can help regulate the body's inflammatory response and mitigate the impact of stress on migraine triggers. Finding healthy coping mechanisms to manage stress is crucial in preventing and managing migraines effectively. Prioritizing activities that promote relaxation and reduce stress can have a positive effect on both mental well-being and overall inflammation levels.
Sleep Deprivation and Its Inflammatory Impact
Adequate sleep is essential for maintaining a healthy inflammatory balance. Sleep deprivation, whether from insufficient hours or poor sleep quality, can disrupt the body's natural inflammatory processes. When we don't get enough sleep, our bodies produce higher levels of inflammatory markers. This increased inflammation can contribute to a range of health problems, including migraines.
Maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a conducive sleep environment can significantly improve sleep quality. Prioritizing sufficient sleep duration and quality can have a positive effect on overall health and help manage inflammation-related migraine episodes.
The Role of Physical Activity in Inflammation
Regular physical activity plays a vital role in modulating inflammation and can have a positive impact on migraine management. Exercise helps to improve blood circulation, reduce stress hormones, and promote the release of endorphins, which have anti-inflammatory properties. Engaging in moderate-intensity aerobic exercises such as brisk walking, jogging, or swimming can help reduce inflammation throughout the body, potentially lessening the frequency and intensity of migraine attacks.
Finding activities you enjoy and incorporating them into your routine is key to long-term adherence. Even short bursts of physical activity throughout the day can contribute to overall health and well-being, potentially impacting inflammation and migraines positively. Consistent physical activity is not only beneficial for reducing inflammation but also for improving overall mood and reducing stress, which can further contribute to migraine management.