Health
Neurology
Migraine Prevention
Medication
HTML
Styling
Medication Interactions
Drug Interactions
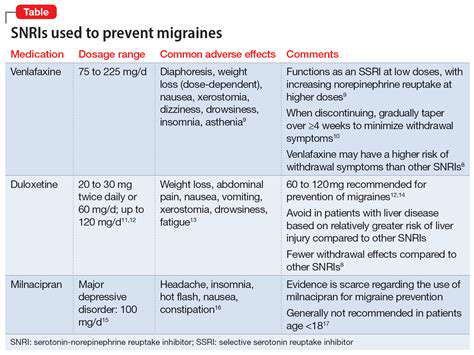
Antidepressivos como estratégia de prevenção da enxaqueca
Uma Relação Complexa

O Impacto da Depressão no Coração
A depressão manifesta-se como algo mais do que sofrimento psicológico – exerce um efeito tangível
Antidepressivos como Estratégia de Prevenção de Enxaquecas: Explorando as Evidências
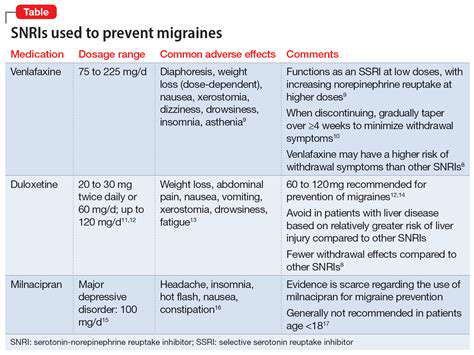
Potenciais Benefícios dos Antidepressivos para a Prevenção da Enxaqueca
Considerações e Limitações Importantes
Interações Medicamentosas
Usuários potenciais de antidepressivos devem considerar as potenciais interações medicamentosas, particularmente para pacientes que tomam múltiplos medicamentos. A consulta profissional ajuda a identificar
Read more about Antidepressivos como estratégia de prevenção da enxaqueca
Entendendo Causas, Sintomas e Tratamentos Explore as causas comuns da dor de cabeça atrás do olho esquerdo, incluindo enxaquecas, sinusite, dores de cabeça em broto e distúrbios nervosos. Este guia abrangente detalha os sintomas a serem observados, opções de tratamento eficazes e quando buscar atendimento médico. Aprenda como modificações no estilo de vida, remédios caseiros e medicamentos de venda livre podem aliviar seu desconforto. Mantenha-se informado sobre sinais graves que requerem consulta médica imediata para garantir o manejo eficaz e uma melhor qualidade de vida. Para aconselhamento personalizado, consulte um profissional de saúde.
Oct 14, 2024
Explore um guia abrangente sobre medicamentos para alívio da dor, com foco em vários tipos disponíveis para a gestão da dor crônica, incluindo opções de venda livre e prescritas. Aprenda sobre anti-inflamatórios não esteroides (AINEs), opioides e medicamentos adjuvantes, como antidepressivos e anticonvulsivantes. Descubra as diferenças entre analgésicos tópicos e remédios naturais, como aromaterapia e terapia de massagem, enquanto também compreende os riscos e benefícios associados a cada opção de tratamento. Envolva-se em estratégias personalizadas de manejo da dor que incorporam mudanças no estilo de vida e terapias emergentes para resultados ótimos. Consulte profissionais de saúde para encontrar as melhores soluções de alívio da dor adaptadas às suas necessidades.
Oct 15, 2024
Melhore sua Postura para uma Melhor Saúde e Bem-Estar. Descubra o impacto da má postura na saúde física e mental. Este guia abrangente explora as causas da má postura - desde estilos de vida sedentários e má ergonomia até dependência da tecnologia e estresse. Aprenda a identificar os sinais de má postura e seus efeitos prejudiciais, incluindo dor crônica, redução da capacidade pulmonar e diminuição da produtividade. Explore soluções práticas, incluindo exercícios específicos, ajustes ergonômicos e práticas de mindfulness projetadas para melhorar a postura e promover o bem-estar geral. Seja você alguém que busca melhorias duradouras na postura ou deseja mitigar os efeitos adversos de longas horas diante do computador, este recurso oferece estratégias acionáveis para um você mais saudável e confiante. Eleve sua postura e aumente sua saúde física e mental hoje!
Oct 17, 2024
//ts2.mm.bing.net/th?q=Causas Comuns da Dor no Lado Direito da Cabeça)
Oct 18, 2024
Atividades envolvendo sobrecarga, postura inadequada ou movimentos repetitivos podem levar à rigidez e dor muscular. Realizar aquecimentos e desaquecimentos adequados é crucial para prevenir a tensão. 2. Estresse Emocional e Ansiedade: O estresse desencadeia uma resposta natural de 'luta ou fuga', resultando em tensão muscular. Cuidar da saúde emocional por meio de terapia e mindfulness pode reduzir significativamente a tensão muscular. 3. Condições Médicas e Lesões: Condições como fibromialgia ou lesões podem levar a uma tensão muscular crônica, à medida que o corpo reage à dor ou desconforto. Compreender essas questões médicas subjacentes é vital para um tratamento eficaz. Consequências da Tensão Muscular Crônica: A tensão muscular crônica pode levar a diversos problemas de saúde física e mental, incluindo dores de cabeça, dores nas costas, ansiedade e mobilidade reduzida. Reconhecer os sintomas, como dores persistentes e fadiga, é essencial para a intervenção precoce. Estratégias de Alívio: Estratégias eficazes de alívio incluem: - Alongamento Regular: Fundamental para melhorar a flexibilidade e reduzir a tensão. - Práticas de Mindfulness: Técnicas como yoga e meditação podem ajudar a aliviar tanto a tensão física quanto a mental. - Nutrição e Hidratação Adequadas: Uma dieta equilibrada com hidratação suficiente desempenha um papel significativo na saúde muscular. Quando Buscar Ajuda: Se você sentir tensão muscular persistente acompanhada de dor ou problemas de mobilidade, é aconselhável consultar um profissional de saúde. Eles podem avaliar sua condição e sugerir intervenções específicas para alívio. Explore mais sobre como gerenciar a tensão muscular para melhorar seu bem-estar geral.
Nov 12, 2024
Gatilhos Comuns da Cefaleia Tensional – Compreensão e Estratégias de PrevençãoMeta Description: Descubra os gatilhos comuns da cefaleia tensional, incluindo estresse, fatores de estilo de vida, influências ambientais e impactos nutricionais. Aprenda estratégias eficazes de prevenção e mudanças no estilo de vida para reduzir a frequência das dores de cabeça e melhorar sua qualidade de vida.Resumo do Conteúdo: Explore os principais gatilhos que contribuem para a cefaleia tensional, desde estresse e má postura até bem-estar emocional e escolhas alimentares. Compreenda como fatores ambientais como ruído e iluminação podem intensificar as dores de cabeça e como ajustes no estilo de vida, como exercícios regulares, uma melhor higiene do sono e práticas de mindfulness podem proporcionar alívio. Além disso, aprenda quando buscar ajuda profissional para dores de cabeça crônicas, com insights sobre opções terapêuticas, como fisioterapia e terapia cognitivo-comportamental. Este guia abrangente tem como objetivo capacitá-lo com conhecimento e estratégias para um gerenciamento eficaz da dor de cabeça.
Nov 13, 2024
Explore a relação intricada entre eventos traumáticos e a saúde do couro cabeludo em nosso artigo abrangente. Descubra como traumas físicos e emocionais podem levar ao aumento da sensibilidade, dor e sensibilidade do couro cabeludo. Analisamos o impacto do estresse psicológico nos sintomas físicos, condições de dor crônica e abordagens de tratamento eficazes. Aprenda sobre estratégias de autocuidado, a importância da consulta profissional e os planos de gestão a longo prazo para aliviar a dor no couro cabeludo. Nosso artigo enfatiza a necessidade de cura holística, abordando tanto o desconforto físico quanto o bem-estar emocional, equipando os leitores com insights valiosos e recursos para a recuperação e prevenção.
Nov 18, 2024
Dor na Parte Superior da Cabeça: Causas e Opções de Tratamento
Apr 30, 2025
Dor nas Costas e na Parte Superior da Cabeça: Possíveis Causas e Soluções
May 02, 2025
Cefaleias em Crianças: Quando se Preocupar e o que Ajuda
May 07, 2025
Cefaleias de tensão: Identificando causas e encontrando alívio
May 15, 2025
Gerenciando Migrañas em um Trabalho de Alto Estresse
May 31, 2025