Health
Neurology
Migraine Prevention
Medication
HTML
Styling
Medication Interactions
Drug Interactions
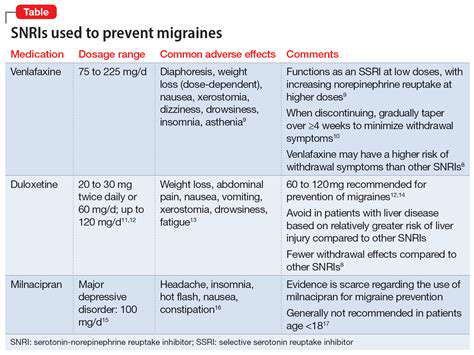
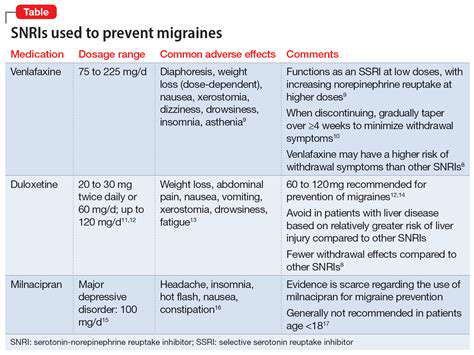
抗憂鬱藥物作為偏頭痛預防策略
複雜的關係

憂鬱症對心臟的影響
憂鬱症不只是心理上的困擾,它也帶來實質性的影響
憂鬱症藥物作為偏頭痛預防策略:探討證據
Read more about 抗憂鬱藥物作為偏頭痛預防策略
了解原因、症狀和治療方法 了解左眼後方頭痛的常見原因,包括偏頭痛、鼻竇炎、叢集性頭痛和神經疾病。本綜合指南詳細介紹了需要注意的症狀、有效的治療選擇,以及何時尋求醫療幫助。了解生活方式改變、家庭療法和非處方藥物如何緩解不適。了解需要立即就醫的嚴重症狀,以確保有效管理和更好的生活品質。如需個性化建議,請諮詢醫療專業人員。
Oct 14, 2024
探索一份全面的止痛藥物指南,重點介紹用於慢性疼痛管理的各種藥物,包括非處方藥和處方藥。了解非類固醇抗炎藥(NSAIDs)、鴉片類藥物以及輔助藥物,如抗憂鬱藥和抗癲癇藥。發現局部止痛劑與香氣治療和按摩治療等自然療法之間的區別,同時了解與每種治療選項相關的風險和好處。參與個性化的疼痛管理策略,結合生活方式的改變和新興療法,以獲得最佳效果。與醫療提供者諮詢,以找到適合您需求的最佳止痛解決方案。
Oct 15, 2024
改善姿勢,提升健康與幸福感。了解不良姿勢對身心健康的影響。本綜合指南探討了不良姿勢的原因——從久坐生活方式和差勁的人體工學到對科技的過度依賴和壓力。學習如何識別不良姿勢的跡象及其危害影響,包括慢性疼痛、肺活量減少和生產力下降。探索實用解決方案,包括針對性鍛煉、人體工學調整和正念練習,以提升姿勢並促進整體健康。無論您是尋求持久改善姿勢,還是希望減輕長時間坐在桌子前的負面影響,這個資源都提供了可行的策略,讓您更加健康、自信。今天就提升您的姿勢,促進身心健康!
Oct 17, 2024
//ts2.mm.bing.net/th?q=右側頭痛的常見原因)
Oct 18, 2024
過度疲勞、不當姿勢或重複運動等活動可能導致肌肉緊繃和酸痛。進行適當的熱身和拉伸對於預防肌肉緊張至關重要。2. 情緒壓力和焦慮:壓力會觸發自然的「戰鬥或逃跑」反應,導致肌肉收緊。通過治療和正念練習關注情緒健康可以顯著減少肌肉緊張。3. 醫療狀況和傷害:纖維肌痛或其他傷害等情況可能導致慢性肌肉緊張,因為身體對疼痛或不適有反應。了解這些潛在的醫療問題對於有效治療至關重要。慢性肌肉緊張的後果慢性肌肉緊張可能導致各種身體和心理健康問題,包括頭痛、背痛、焦慮和活動能力下降。識別持續的疼痛和疲憊等症狀對於早期干預至關重要。緩解策略有效的緩解策略包括:- 定期拉伸:改善靈活性和減少緊張的關鍵。- 正念練習:瑜伽和冥想等技術可以幫助緩解身體和心理的緊張。- 合理的營養和水分攝入:均衡的飲食和充足的水分對肌肉健康起著重要作用。何時尋求幫助如果你經歷持續的肌肉緊張伴隨疼痛或活動能力問題,建議諮詢醫療專業人士。他們可以評估你的狀況並建議有針對性的緩解干預。進一步探索管理肌肉緊張的方法,以改善整體健康。
Nov 12, 2024
緊張性頭痛的常見誘因 – 理解與預防策略Meta Description: 發現緊張性頭痛的常見誘因,包括壓力、生活方式因素、環境影響和營養影響。學習有效的預防策略和生活方式改變,以減少頭痛頻率並改善生活品質。內容摘要: 探索導致緊張性頭痛的主要誘因,從壓力和不良姿勢到情緒健康和飲食選擇。了解噪音和光照等環境因素如何加劇頭痛,以及規律運動、改善睡眠衛生和正念練習等生活方式調整如何提供緩解。此外,了解何時尋求專業幫助以應對慢性頭痛,以及物理治療和認知行為療法等治療選擇的見解。本綜合指導旨在通過知識和策略使您掌握有效的頭痛管理。
Nov 13, 2024
在我們的綜合文章中探討創傷事件與頭皮健康之間複雜的關係。發現身體和情感創傷如何導致頭皮敏感性、疼痛和壓痛的增加。我們深入探討心理壓力對身體症狀、慢性疼痛情況及有效治療方法的影響。了解自我護理策略、專業諮詢的重要性以及緩解頭皮疼痛的長期管理計畫。我們的文章強調通過解決身體不適和情感健康來實現整體療癒的必要性,為讀者提供有價值的洞見和恢復與預防的資源。
Nov 18, 2024