Beta Blockers for Migraine Prevention: An Overview
Types of Beta-Blockers Commonly Used
Cardioselective Beta-Blockers
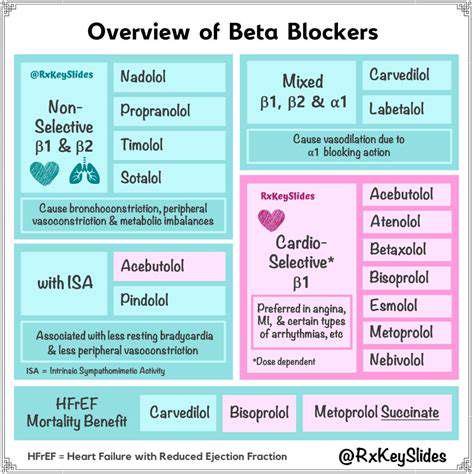
Cardioselective beta-blockers, such as metoprolol and bisoprolol, primarily affect beta-1 adrenergic receptors in the heart. This selectivity typically leads to fewer side effects on the lungs and bronchioles compared to non-selective beta-blockers. These medications are often a first-line choice for patients with conditions like angina, hypertension, and certain types of arrhythmias, as they can effectively reduce heart rate and contractility without significantly impacting respiratory function. They are generally well-tolerated, though individual responses can vary.
The precise mechanism of action involves blocking the binding of norepinephrine and epinephrine to beta-1 receptors, thus reducing the sympathetic nervous system's influence on the heart. This results in a decrease in heart rate, blood pressure, and force of contraction, ultimately lowering the workload on the heart.
Non-Selective Beta-Blockers
Non-selective beta-blockers, like propranolol and nadolol, affect both beta-1 and beta-2 adrenergic receptors. While this broader action can be beneficial in certain situations, it also increases the risk of side effects, particularly in individuals with pre-existing respiratory conditions. This is because beta-2 receptors are crucial for bronchodilation, and blocking them can lead to bronchospasm, making breathing difficult.
These medications are often used in conditions where a more comprehensive reduction in sympathetic activity is desired, such as severe hypertension, some types of arrhythmias, and essential tremor. However, their use needs to be carefully considered in patients with asthma or chronic obstructive pulmonary disease (COPD) due to the potential for adverse respiratory effects.
Beta-1 Selective Beta-Blockers
Beta-1 selective beta-blockers, as mentioned previously, primarily target beta-1 receptors in the heart. This focused action minimizes the impact on other systems, such as the lungs. This targeted approach makes them a preferred choice for patients with conditions that primarily affect the cardiovascular system. This focused action is crucial in reducing the risk of unwanted side effects, particularly those related to respiratory function.
These medications are commonly prescribed for conditions like hypertension, angina, and certain types of arrhythmias. Their selectivity reduces the likelihood of adverse effects on the airways, making them a safer option for patients with pre-existing respiratory conditions compared to non-selective beta-blockers.
Beta-Blockers with Intrinsic Sympathomimetic Activity
Some beta-blockers, like acebutolol and penbutolol, possess intrinsic sympathomimetic activity. This means they have a partial agonist effect on beta receptors. They can reduce heart rate and blood pressure, but to a lesser extent than non-selective beta-blockers. This reduced effect on heart rate and blood pressure can be advantageous in patients who experience significant bradycardia with other beta-blockers.
This characteristic can result in a milder reduction in heart rate and blood pressure, which can be beneficial in certain patients. However, the overall efficacy may not be as robust as with other beta-blocker types. The presence of intrinsic sympathomimetic activity might also be less desirable in situations requiring a substantial decrease in sympathetic activity.
Beta-Blockers and their Specific Indications
Various beta-blockers are used for a range of cardiovascular conditions. For instance, metoprolol succinate is frequently prescribed for chronic hypertension, while propranolol is sometimes utilized for migraines and essential tremor. The choice of beta-blocker depends on the individual patient's needs and health status. It's crucial to consult with a healthcare professional to determine the most suitable beta-blocker for a particular condition.
Understanding the specific indications and potential side effects of each beta-blocker is essential for appropriate patient management. This information helps clinicians tailor treatment strategies to optimize patient outcomes and minimize adverse effects. The selection of the appropriate beta-blocker is a personalized decision, considering individual patient characteristics and medical history.
Beta-Blockers and their Dosage Considerations
Dosage considerations for beta-blockers are crucial for achieving therapeutic efficacy while minimizing potential side effects. The dosage regimen is typically adjusted based on the individual patient's response, blood pressure readings, and the specific condition being treated. Precise dosage is essential to avoid both under-treatment and over-treatment.
Factors such as age, weight, and concomitant medications can influence the required dosage. Close monitoring of the patient's response to the medication is crucial during the initial stages of treatment and throughout the course of therapy. Adjusting the dosage as needed allows for optimized outcomes while minimizing potential complications.
Alternatives and Considerations
Non-Pharmacological Approaches
While medication is often a crucial component of migraine prevention, Non-pharmacological strategies can significantly complement or even replace medication for some individuals. These approaches often address the root causes of migraines, such as stress, sleep deprivation, and dietary triggers. Identifying and managing these factors can dramatically reduce the frequency and intensity of migraine attacks. Lifestyle modifications like maintaining a regular sleep schedule, stress reduction techniques (yoga, meditation, or mindfulness), and a balanced diet rich in fruits, vegetables, and lean proteins can play a pivotal role in migraine prevention.
Other Medications
Beyond beta-blockers, other medications can be considered for migraine prevention. Triptans, for instance, are often used to treat acute migraine attacks but can also be prescribed for preventative use in some cases. CGRP inhibitors are another class of medications gaining popularity for migraine prevention. These medications work by targeting a specific protein in the nervous system involved in migraine pain. The choice of medication, whether beta-blocker, triptan, or CGRP inhibitor, should be made in consultation with a healthcare professional.
Individualized Treatment Plans
Migraine is a complex condition, and the effectiveness of beta-blockers, or any other medication, varies significantly from person to person. A personalized treatment plan is therefore crucial. This involves careful consideration of individual factors, including the frequency, intensity, and triggers of migraines, as well as the patient's overall health and any other medications they may be taking. The healthcare professional must carefully weigh the potential benefits and risks of each treatment option to determine the most appropriate course of action.
Monitoring and Adjustment
Once a treatment plan is established, ongoing monitoring is essential. Regular follow-up appointments allow for evaluation of the effectiveness of the treatment and adjustments as needed. It's crucial to communicate openly with your healthcare provider about any changes in the frequency, intensity, or characteristics of your migraines. This feedback loop ensures that the treatment strategy remains optimal and addresses any emerging needs.
Lifestyle Considerations and Patient Education
Beyond medication, a crucial aspect of migraine prevention involves lifestyle modifications. This includes maintaining a regular sleep schedule, managing stress effectively, and identifying and avoiding dietary triggers. Patient education plays a vital role in empowering individuals to take an active part in their migraine prevention. Understanding the triggers, recognizing the warning signs, and adopting healthy habits are all key components of a comprehensive approach to migraine management.