How to Support a Loved One Who Suffers from Migraines
Communicating Effectively and Empathetically
Understanding the Impact of Suffering
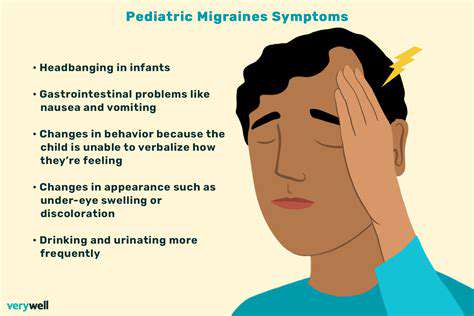
Suffering, in its many forms, can profoundly impact a person's emotional well-being, influencing their thoughts, feelings, and behaviors. Recognizing that suffering is deeply personal and unique to each individual is the first step toward meaningful support. Whether it manifests as anxiety, depression, or physical pain, understanding these nuances is key to offering genuine help.
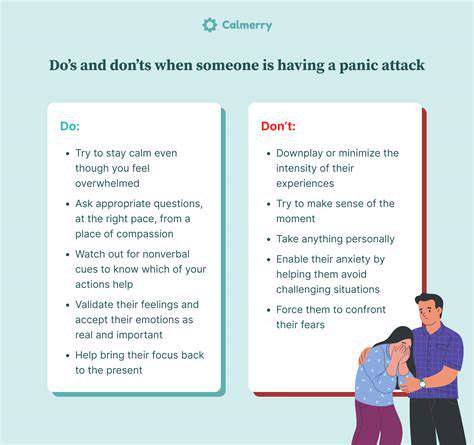
Approach conversations with empathy and patience. Avoid dismissing their experience, even if it’s unfamiliar to you. Simply acknowledging their feelings—without offering unsolicited advice—can make a world of difference.
Active Listening and Validation
Active listening is more than just hearing words; it’s about understanding the emotions behind them. Pay attention to nonverbal cues like body language and tone, which often reveal more than words alone. Validation—acknowledging their feelings without judgment—is a cornerstone of effective support. Phrases like, This sounds incredibly hard for you, or Your feelings make sense, can foster trust and connection.
Offering Practical Support
Emotional support is vital, but practical help can be equally impactful. Small gestures—like running errands, cooking a meal, or helping with childcare—can alleviate daily stressors. Ask directly, What would help you most right now? This ensures your efforts align with their actual needs rather than assumptions.
Setting Boundaries and Self-Care
Supporting someone in distress can be draining. Protect your own well-being by setting clear boundaries and prioritizing self-care. Regular breaks, hobbies, or time with friends recharge your emotional reserves, enabling you to give sustained support without burnout.
Respecting Their Choices
Resist the urge to fix their problems. Everyone copes differently, and what works for you may not work for them. Instead, empower them by respecting their autonomy. Trust that they know their needs best, even if their path differs from yours.
Honest Communication
Create a safe space for open dialogue. Encourage them to share freely, and respond with honesty and compassion. Effective communication is a two-way street—listen as much as you speak.
Seeking Professional Help
If their suffering feels overwhelming, gently suggest professional support. Therapists or support groups offer specialized tools for healing. Your role isn’t to replace experts but to guide them toward additional resources.
Creating a Supportive Environment: Practical Accommodations
Understanding Their Needs
Start by asking, What would make things easier for you? Observe their reactions and preferences to tailor your support. Avoid assumptions—what helps one person might overwhelm another.
Communication Strategies
Use I statements to express care without pressure. For example, I’d like to help—would it be okay if I...? This keeps the focus on collaboration, not control.
Practical Adjustments
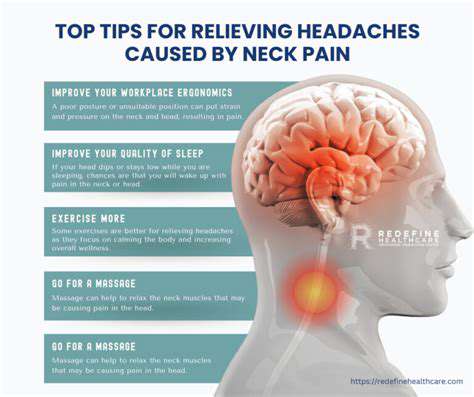
Modify their environment to reduce stressors. This could mean dimming lights for migraines or creating a quiet space for anxiety. Small changes often yield significant relief.
Emotional Validation
Sometimes, the best support is silent presence. A simple, I’m here with you, can be more powerful than solutions.
Professional and Community Resources
Don’t hesitate to involve experts or support groups. Shared experiences and professional guidance can fill gaps that personal support alone cannot.
Practical Support During an Attack: What to Do and Avoid
Recognizing the Attack
Understanding the attack’s nature is critical. Is it sensory overload, pain flare-ups, or emotional distress? Identifying triggers helps tailor your response.
Immediate Actions
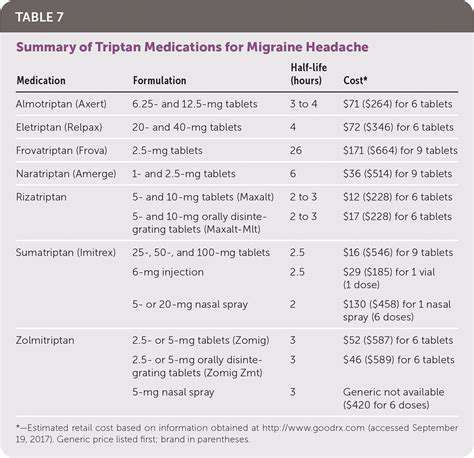
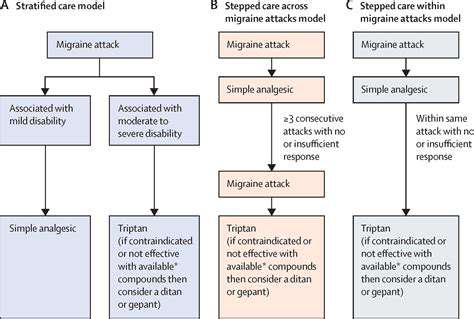
Stay calm and ask, How can I help right now? Quick, simple actions—like fetching medication or reducing noise—can mitigate severity. Avoid overwhelming them with questions.
Long-Term Strategies
Work together to identify patterns and preventative measures. Consistency in support—like maintaining a symptom journal—builds resilience over time.
Recovery and Preparedness
After an attack, debrief gently. What helped or didn’t help? Use these insights to refine future responses, turning crises into learning opportunities.