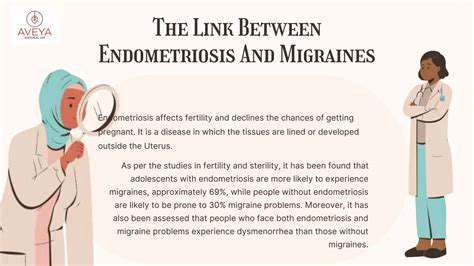
Exploring Endometriosis and Increased Migraine Risk
Impact on Reproductive Health
Endometriosis profoundly affects fertility through multiple mechanisms. The inflammatory environment created by ectopic tissue damages reproductive structures. Scar tissue can distort pelvic anatomy, while inflammatory chemicals may impair egg quality, fertilization, and embryo implantation. While pregnancy remains possible, affected women often face greater challenges conceiving and higher risks of complications like ectopic pregnancy.
Treatment Options for Endometriosis
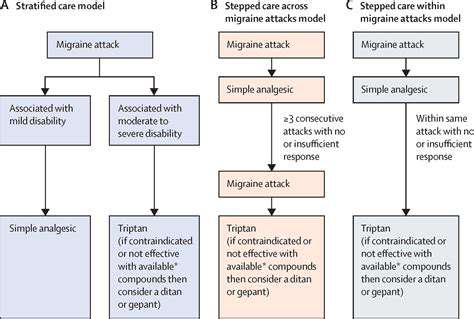
Treatment strategies must be personalized based on symptom severity and reproductive goals. First-line approaches focus on symptom control while preserving fertility potential. Options range from NSAIDs for pain management to hormonal therapies (oral contraceptives, progestins, or GnRH agonists) that suppress endometrial growth. Many patients benefit from complementary approaches like physical therapy, acupuncture, or anti-inflammatory diets.
Surgical options include laparoscopic excision of lesions or, in severe cases, hysterectomy. Emerging treatments target specific inflammatory pathways or utilize novel drug delivery systems. The optimal approach requires careful discussion with a specialist who understands both medical and quality-of-life considerations.
Living with Endometriosis: Support and Management
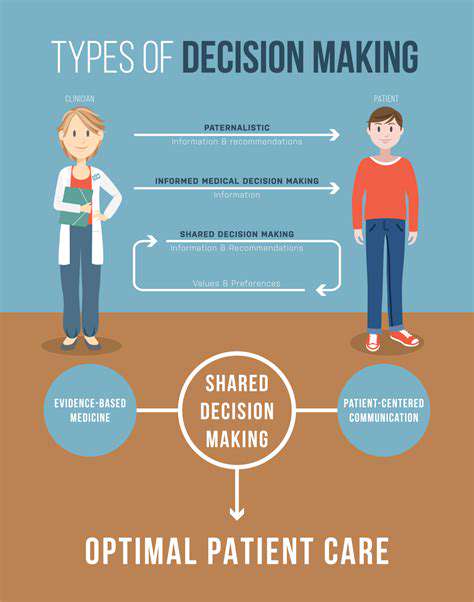
Effective endometriosis management requires a comprehensive, multidisciplinary approach. Building a strong support network of healthcare providers, patient communities, and understanding loved ones proves crucial for long-term coping. Many patients find relief through stress-reduction techniques like mindfulness meditation, yoga, or cognitive behavioral therapy. Maintaining detailed symptom journals helps identify triggers and track treatment effectiveness.
Regular specialist follow-ups allow for timely treatment adjustments. Some patients benefit from working with pain management specialists or reproductive endocrinologists. Staying informed about emerging research empowers patients to advocate for their care and explore new options as they become available.
Consider this revealing exercise: Document your five most productive work moments. Analyze the circumstances - location, time of day, environmental factors. Many discover their optimal work environment differs dramatically from traditional expectations. For instance, architect Maria found her best designs emerged during early morning sessions in her home office, contrary to her firm's open-plan workspace.
Potential Inflammatory Mechanisms
Potential Inflammatory Mediators
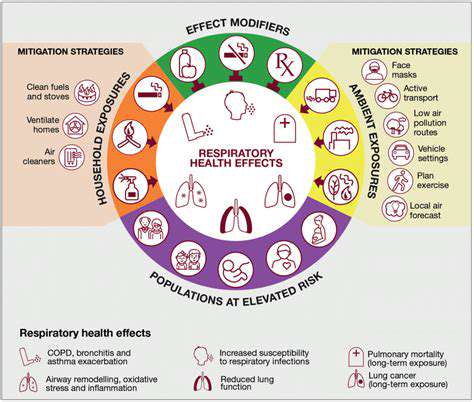
Chronic inflammation drives endometriosis progression through complex molecular interactions. The ectopic tissue secretes inflammatory factors that recruit immune cells and stimulate nerve growth, creating a self-perpetuating cycle of pain and tissue damage. Researchers continue identifying novel mediators that could serve as therapeutic targets.
Role of Cytokines in Endometriosis
Key inflammatory cytokines like IL-1β, TNF-α, and IL-8 show elevated levels in endometriosis patients. These molecules not only promote inflammation but also stimulate angiogenesis (new blood vessel formation) that supports ectopic tissue survival. Some experimental treatments specifically target these cytokine pathways to interrupt disease progression.
Endometriosis-Associated Oxidative Stress
The inflammatory environment generates excessive reactive oxygen species that overwhelm natural antioxidant defenses. This oxidative stress damages cells and DNA, potentially contributing to disease persistence and associated infertility. Some clinicians recommend antioxidant supplementation as part of comprehensive treatment plans.
The Impact of Immune Cells
Macrophages and other immune cells display altered function in endometriosis patients. Instead of clearing ectopic tissue, they often promote its survival through growth factor secretion. Regulatory T-cell dysfunction may explain why the immune system fails to eliminate misplaced endometrial cells. Immunomodulatory approaches represent an exciting frontier in endometriosis research.
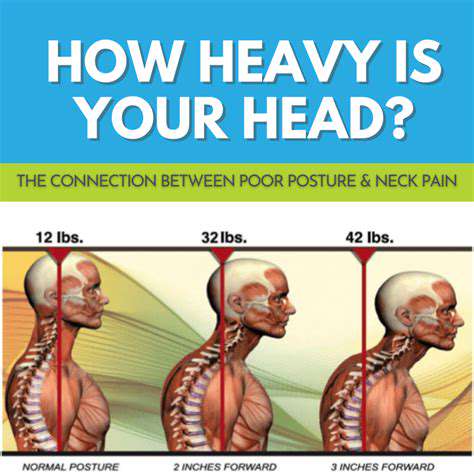
Neurogenic Inflammation and Endometriosis
Nerve fibers infiltrating endometriosis lesions release substance P and other neuropeptides that amplify inflammatory responses. This neuro-immune crosstalk contributes to the characteristic chronic pain. Some newer medications specifically target these neural pathways to provide more effective pain relief.
The Role of the Endometrial Microenvironment
The surrounding stromal cells and extracellular matrix create a supportive niche for ectopic tissue through complex signaling networks. Hypoxia (low oxygen) in these lesions triggers adaptive responses that promote survival. Understanding these microenvironmental factors could lead to therapies that disrupt the supportive niche.
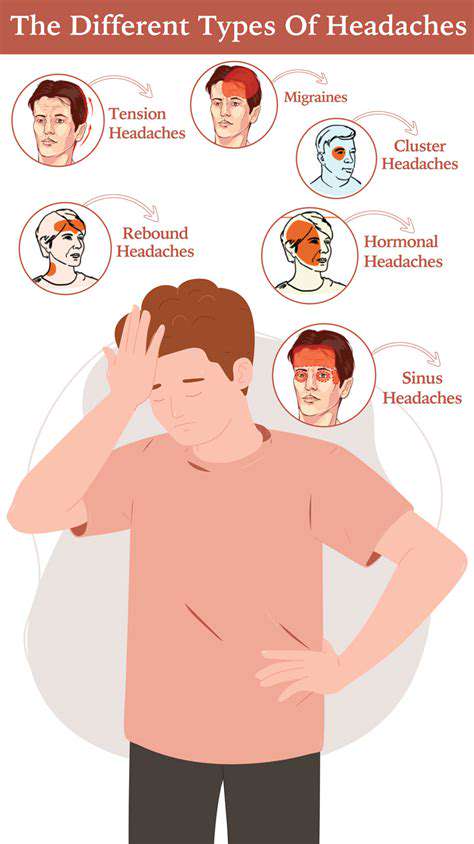
Potential Link to Migraine Pathogenesis
The shared inflammatory pathways between endometriosis and migraines may explain their frequent co-occurrence. Both conditions involve elevated prostaglandins and similar cytokine profiles. Some migraine medications show promise for endometriosis pain, suggesting potential therapeutic overlap worth further exploration.