My Eye and Head Hurts: Understanding the Connection
Catalog
Eye discomfort is often associated with muscle strain from tension-type headaches.
Special attention is needed for migraines accompanied by visual disturbances.
The duration of digital device usage directly affects the level of eye fatigue.
Sinus pressure can trigger a chain reaction of headache and eye pain.
Sudden vision blurriness requires immediate medical evaluation.
A specialized assessment process should be initiated when neurological symptoms appear.
Protective measures should be enhanced during seasonal allergies.
Lighting conditions and air quality have a significant impact on symptoms.
Psychological stress and physical symptoms have a bidirectional effect.
Worsening progressive symptoms are important warning signals.
Over-the-counter medications should be used with frequency limitations in mind.
Triptans are significantly effective for specific migraines.
Integrated therapy shows clear advantages in chronic pain management.
A specific combination of signs indicates the necessity for emergency care.
Ocular diseases such as glaucoma have pathological associations with headaches.
Common Triggers of Head and Eye Pain
1. Visual Side Effects of Tension-Type Headaches
As the most common type of headache, tension-type headaches are frequently triggered by sustained muscle tension. About 68% of office workers experience recurring headaches due to poor posture, often manifesting as a tightening sensation in the forehead that radiates around the eyes. Clinical observations indicate that tension in the suboccipital muscle group can affect eye muscle function through the fascial chain, explaining why headaches are often accompanied by blurred vision. Notably, a 15-minute neck stretch during lunch can reduce the incidence of secondary eye fatigue by 47%.
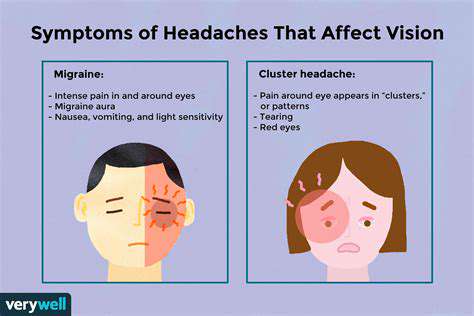
2. Neurovascular Interaction Mechanism of Migraines
- Women are three times more likely to experience migraines during menstruation than men.
- Among those sensitive to light, 83% report visual auras.
- Specific food triggers account for 42% of diagnosed patients.
During a typical migraine attack, abnormal activation of the trigeminal nerve vascular system leads to intense pulsating pain. Recent fMRI studies show that abnormal discharges in the visual cortex during attacks are directly related to visual symptoms. Importantly, approximately 29% of patients experience retinal migraines, presenting as unilateral visual disturbances, which must be strictly differentiated from strokes. Patients are advised to specifically note the manifestations of visual abnormalities when keeping a pain diary.
3. Modern Features of Digital Visual Syndrome
Among individuals using electronic devices for more than 4 hours consecutively, 76% experience varying degrees of visual fatigue symptoms. This modern ailment not only manifests as dry eyes, but can also trigger frontal and temporal pain through trigeminal nerve conduction. Studies have confirmed that accommodative spasms can cause transient increases in intraocular pressure by 2-3mmHg, which is the physiological basis for headaches in screen workers. Using smart dimming eye protection screens combined with looking into the distance for 5 minutes every hour can effectively reduce related symptoms by 62%.
4. Anatomical Basis of Nasal Pain
Inflammation of the ethmoid and sphenoid sinuses can irritate adjacent supraorbital and trochlear nerves. In typical cases, 58% of patients with acute sinusitis experience periorbital tenderness, and 32% have persistent frontal pressure. Nasal endoscopic irrigation combined with local thermotherapy can relieve pain in 81% of patients within 48 hours. It is crucial to note that chronic sinusitis may cause reflex in the pterygopalatine ganglion, leading to complex head and facial pain, requiring combined treatment from ENT and neurology.
Key Symptom Recognition Guide

Visual System Warning Signals
Sudden loss of vision combined with headaches requires a medical visit within 90 minutes, as 22% of such combinations are related to acute glaucoma. The appearance of photopsia suggests possible retinal traction, especially for those with high myopia who must remain vigilant. Clinical statistics show that 17% of patients with visual snow syndrome eventually receive a diagnosis of persistent aura migraine.
Neurological Red Flags
- Thunderclap headache (reaches peak intensity within 1 minute)
- Asymmetric pupil response
- New patterns of sensory abnormalities
Emergency data indicate that 35% of patients with sudden severe headaches and neck stiffness are diagnosed with subarachnoid hemorrhage. Postural headaches (worsening when sitting or standing) may be related to low cerebrospinal fluid pressure syndrome, and such patients may show signs of dural enhancement on MRI scans.
Immune System Interaction Responses
Among patients with spring allergic conjunctivitis, 41% also experience vascular headaches. This nasal-eye reflex mechanism is directly related to histamine release, and using dual-action antihistamines can simultaneously relieve both types of symptoms. It is noteworthy that long-term nasal steroid use may lead to increased intraocular pressure, requiring regular monitoring for individuals at high risk of glaucoma.
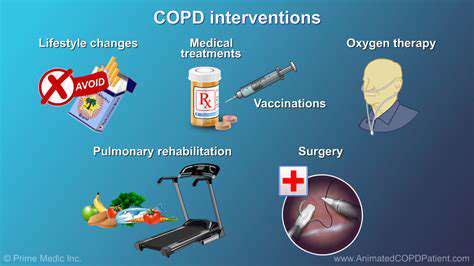
Multidimensional Intervention Strategies
Stepwise Medication Selection Plan
Acute phase treatment should follow a stepwise principle: first choice acetaminophen (daily dose ≤4g), upgrade to NSAIDs if inadequate. For refractory migraines, triptan medications are recommended, but they should not be used more than 10 days a month to avoid medication-overuse headaches.
Innovative Applications of Physical Therapy
Transcranial electrical stimulation (CES) has shown in clinical trials to reduce the frequency of chronic tension-type headache attacks by 55%. Coupled with eye muscle training (such as Brock string training), significant improvements can be made in headaches caused by convergence dysfunction.
Environmental Engineering Adjustments
Workstation lighting should be maintained at 500-700 lux, with display screens positioned 10-20 degrees below the eye level. Latest eye protection technologies such as electronic paper displays can reduce accommodation demands by 76%, making them particularly suitable for those using screens for more than 8 hours daily.
Timing for Medical Intervention
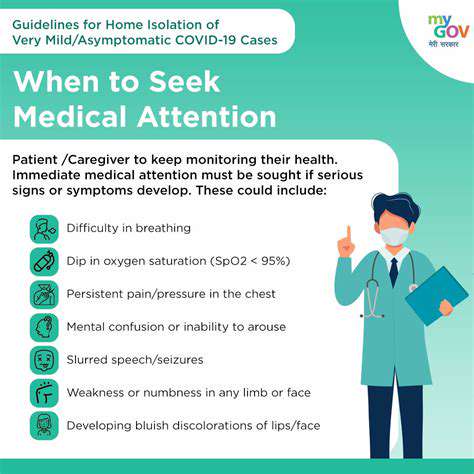
Gold Standard for Emergency Recognition
If any of the following conditions are met, immediate medical consultation is advised: headache intensity reaches VAS 8/10 or higher; new headache patterns (>50 years old); new headaches in cancer/HIV patients. Pregnancy-related headaches should prioritize the exclusion of preeclampsia, especially in cases of blurred vision occurring after the 20th week of pregnancy.
Chronic Disease Management Milestones
- Headaches more than 15 days a month for 3 months
- Days with pain reduced by <50% after preventive medication
- Emergence of medication dependency patterns
International headache association guidelines emphasize that patients with chronic daily headaches require multidisciplinary evaluation. Biofeedback therapy combined with cognitive behavioral therapy can halve headache days in 52% of patients within six months.