New Daily Persistent Headache (NDPH): What You Should Know
Treatment Options and Management Strategies
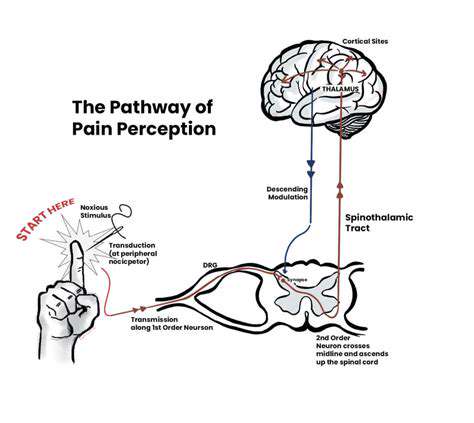
Because NDPH varies so much between patients, treatment plans require careful customization. Some respond well to specific medications, while others benefit more from nerve blocks or physical therapy. Many doctors recommend combining approaches - for instance, pairing preventive medications with stress-reduction techniques.
The most effective treatments address both the physical pain and its emotional impacts. This might involve a neurologist for medication management, a psychologist for coping strategies, and a physical therapist for posture correction. Regular follow-ups allow for adjustments as the condition evolves.
Impact on Daily Life and Quality of Life
Living with NDPH means constantly negotiating with pain. Simple pleasures like reading or socializing become exhausting when your head constantly hurts. Many patients describe feeling trapped in their own bodies, watching life happen around them while they struggle to participate.
The emotional toll often matches the physical suffering, with many patients experiencing depression or anxiety. Relationships strain under the weight of chronic pain, and careers often suffer. Comprehensive treatment must address these quality-of-life issues alongside pain management.
Role of Lifestyle Factors
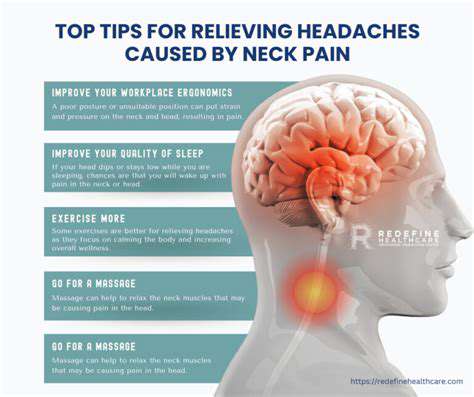
While lifestyle changes won't cure NDPH, they can significantly improve symptom management. Establishing regular sleep patterns helps some patients, while others find relief through gentle yoga or meditation. Dietary adjustments like reducing caffeine or MSG sometimes lessen headache intensity.
Small, consistent lifestyle tweaks often yield better results than drastic overhauls. The key is finding sustainable changes that fit individual circumstances - perhaps swapping one coffee for herbal tea, or taking short walking breaks during work. These modest adjustments can cumulatively make days more manageable.
Seeking Professional Help and Support
If you've had daily headaches for months, don't dismiss them as normal. Primary care physicians can initiate evaluation, but neurologists specializing in headache disorders offer the most expertise. Early specialist involvement often prevents months of ineffective treatments.
Online communities provide invaluable support, offering practical tips and emotional understanding. Many patients find comfort connecting with others who truly grasp what living with constant head pain means. These networks often share resources about new treatments or understanding doctors.

Clear communication becomes even more crucial when working remotely, where the absence of physical cues increases misunderstanding risks. Teams must develop new norms - perhaps scheduling regular video check-ins or using emojis to convey tone in messages. These adaptations help bridge the gap created by physical separation.
Living with NDPH: Coping Strategies and Support

Understanding the Challenges of NDPH
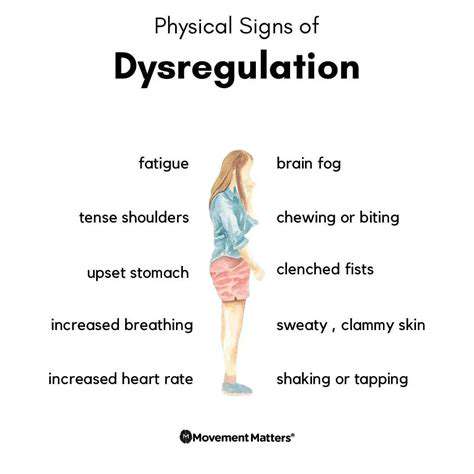
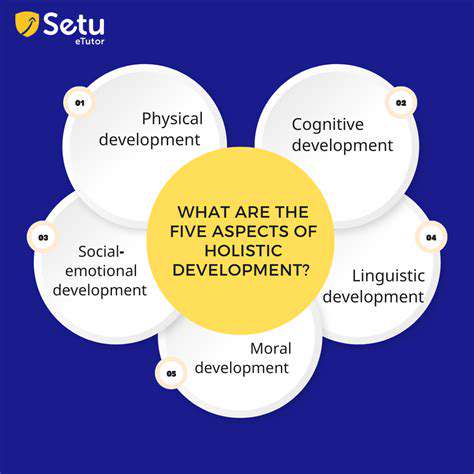
NDPH creates a unique set of obstacles that extend beyond physical pain. Developing effective coping mechanisms requires acknowledging both the visible and invisible struggles. The condition's unpredictability - good days suddenly turning bad - makes planning difficult and fosters anxiety.
Many patients describe grieving their pre-headache lives while adapting to new limitations. This emotional processing is natural but benefits from professional guidance. Cognitive behavioral therapy techniques often help reframe negative thought patterns about the condition.
Developing a Personalized Hydration Plan
While hydration might seem straightforward, NDPH patients often need tailored approaches. Some find relief through electrolyte-enhanced waters, while others benefit from scheduled sipping rather than large volumes at once. Tracking intake alongside headache intensity can reveal surprising patterns.
Neurologists sometimes recommend hydration apps or simple journaling to monitor trends. The goal isn't perfection but understanding how fluid intake interacts with headache symptoms for that individual. Small adjustments based on these observations can yield noticeable improvements.
Utilizing Medication Effectively
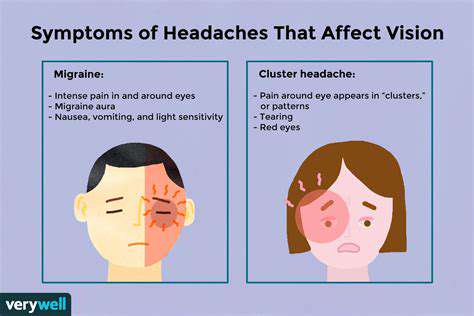
Medication regimens for NDPH often involve trial and error. Some patients respond well to traditional migraine preventatives, while others need more unconventional approaches. Consistency matters tremendously - skipping doses frequently undermines treatment efficacy.
Using pill organizers or smartphone reminders helps maintain medication schedules. Patients should document side effects thoroughly, as this information guides doctors in fine-tuning prescriptions. Never discontinue medications abruptly without medical supervision.
Prioritizing Regular Medical Checkups
Routine monitoring becomes especially important with chronic conditions like NDPH. Beyond standard checkups, many patients benefit from periodic neurological evaluations to assess treatment effectiveness. These appointments also provide opportunities to discuss new research or emerging therapies.
Pre-appointment preparation - writing down questions and symptom updates - maximizes limited consultation time. Bringing a trusted friend or family member can provide emotional support and help remember medical advice.
Building a Support Network
Chronic pain isolates, making community connections vital. Local support groups offer face-to-face understanding, while online forums provide 24/7 access to shared experiences. Some patients find mentoring relationships helpful - connecting with someone further along in their NDPH journey.
Educating close friends and family about the condition prevents misunderstandings. Simple explanations about good days versus bad days help loved ones provide appropriate support without overprotecting or underestimating the challenges.
Adopting Healthy Lifestyle Practices
Wellness strategies should enhance life, not become additional burdens. Instead of drastic diet changes, patients might focus on consistent meal timing. Gentle movement like swimming or tai chi often proves more sustainable than intense workouts. Quality sleep matters more than strict adherence to arbitrary bedtime rules.
Many patients discover unexpected triggers through mindful experimentation - perhaps certain lighting conditions or weather patterns worsen symptoms. Identifying and accommodating these personal sensitivities can significantly improve daily functioning.