Mindfulness Based Stress Reduction (MBSR) for Migraineurs
The Role of the Nervous System
Our nervous system acts as the central conductor orchestrating both stress responses and migraine experiences. Prolonged stress can hypersensitize the trigeminal nerve - the primary highway for pain signals to the brain. Once sensitized, this nerve begins interpreting even minor stressors as significant threats, lowering the threshold for migraine attacks.
Moreover, stress triggers a neurochemical cascade that influences nerve activity and brain function. These biochemical messengers can initiate inflammatory processes frequently observed during migraine episodes. Grasping how stress rewires nervous system function proves essential for understanding migraine susceptibility.
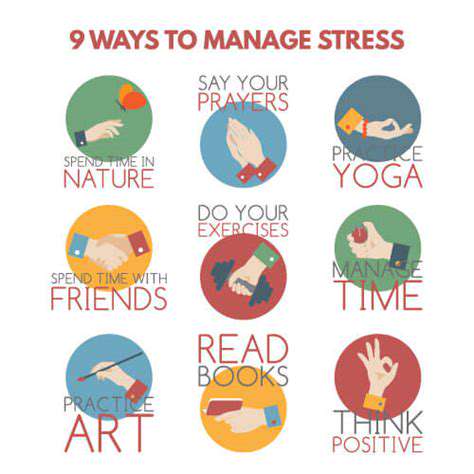
Stress Management Techniques for Migraine Prevention
Given the undeniable stress-migraine relationship, adopting effective stress reduction strategies can dramatically decrease migraine occurrence and severity. Mindfulness techniques like meditation and controlled breathing help individuals regain command over their stress responses. These practices promote deep relaxation, counteracting stress's physiological impacts and reducing migraine triggers.
Additional protective measures include consistent physical activity, prioritizing sleep hygiene, and maintaining balanced nutrition. These lifestyle pillars build overall resilience, creating a buffer against stress-induced migraines.
Mindfulness and its Impact on Migraine Relief
The practice of mindfulness - cultivating nonjudgmental present-moment awareness - demonstrates remarkable potential for stress reduction and migraine management. By developing acute awareness of bodily sensations and emotional states, individuals gain tools for emotional regulation. This skill proves particularly valuable for intercepting stress before it escalates into full-blown migraine pain.
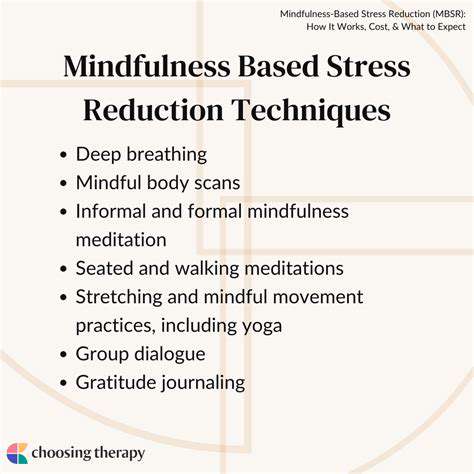
Structured programs like Mindfulness-Based Stress Reduction (MBSR) provide systematic training in mindfulness techniques. Through guided exercises including body scans, seated meditation, and mindful movement, participants develop sustainable strategies for maintaining calm amidst life's stressors.
Seeking Professional Help
While self-care strategies offer substantial benefits, those experiencing frequent or severe migraines should consult healthcare professionals. Physicians can identify specific triggers, recommend personalized treatment plans, and exclude other medical conditions mimicking migraine symptoms.
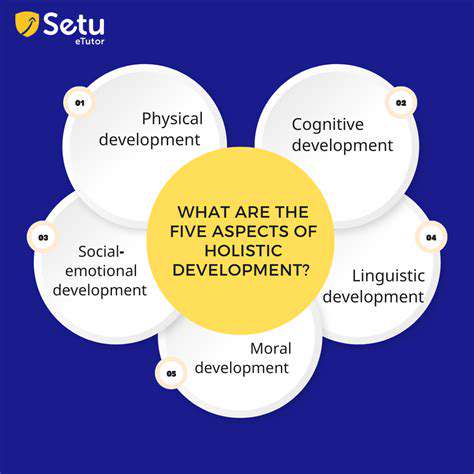
Psychological support also plays a crucial role. Therapists can address the emotional roots of stress and teach comprehensive coping mechanisms, creating a holistic approach to migraine management.
Beyond the Headache: The Holistic Approach of MBSR
Understanding the Root Causes
Headaches represent more than temporary discomfort - they're often warning signals of deeper imbalances. Potential contributors range from simple dehydration to complex health conditions. Pinpointing these underlying factors transforms headache management from symptom suppression to root-cause resolution.
Daily habits significantly influence headache patterns. Irregular sleep, insufficient water intake, and dietary choices can all serve as silent headache triggers, making lifestyle evaluation essential for prevention.
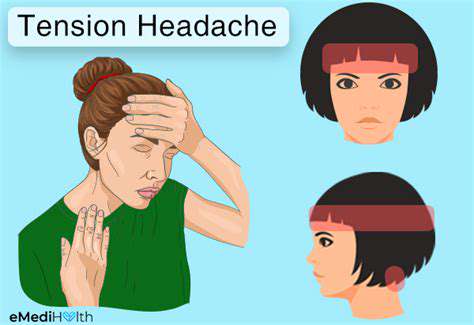
The Role of Stress and Anxiety
Stress and anxiety frequently operate as hidden architects behind both tension headaches and migraines. The body's stress response - with its characteristic muscle tension and hormonal surges - directly paves the way for headache development. Chronic stress creates particularly fertile ground for recurrent headaches.
Mind-body techniques like mindfulness meditation and diaphragmatic breathing can disrupt this cycle. Consistent practice rewires stress responses, offering long-term protection against stress-related headaches.
Dietary Influences and Triggers
Food sensitivities represent highly individualized headache triggers. While some individuals react to caffeine withdrawal, others respond to tyramine-rich foods, nitrates, or artificial sweeteners. Maintaining a detailed headache-food journal helps identify personal dietary triggers, enabling targeted elimination strategies.
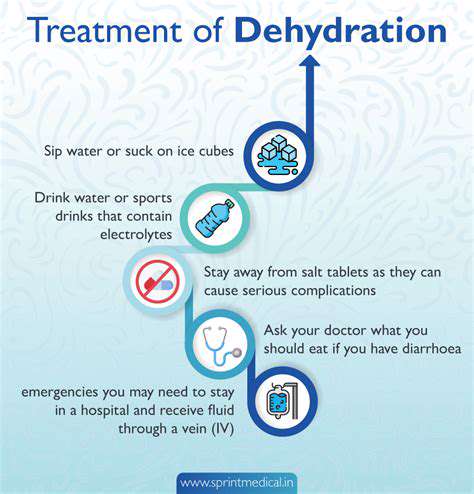
The Importance of Hydration and Sleep
Water constitutes our most basic yet frequently neglected headache prevention tool. Dehydration triggers vascular changes that directly contribute to headache development. Consistent hydration maintains physiological balance and prevents this common trigger.
Sleep quality similarly impacts headache susceptibility. Sleep deprivation elevates stress hormones and muscular tension - both established headache precursors. Prioritizing sufficient, quality sleep creates powerful protection against recurrent headaches.
The Connection to Environmental Factors
External elements like barometric pressure shifts or strong odors can initiate headache cycles through vascular changes. Recognizing these environmental triggers enables proactive avoidance strategies.
The Significance of Physical Activity
Regular exercise delivers multiple headache-prevention benefits. Physical activity modulates stress responses, improves circulation, and reduces muscular tension. Establishing consistent movement patterns can significantly reduce headache frequency and intensity.
Seeking Professional Guidance
While lifestyle modifications help many headache sufferers, professional evaluation becomes crucial when headaches persist or intensify. Persistent or unusual headache patterns may indicate underlying conditions requiring medical attention. Healthcare providers can offer accurate diagnosis and tailored treatment plans.