Pediatric Migraines: Understanding Headaches in Children
Recognizing the Early Signs
Spotting the initial symptoms of pediatric migraines requires careful attention to subtle changes in a child's behavior or complaints. Catching these signs early can dramatically improve outcomes, allowing for quicker intervention and better pain management. Parents might notice their child becoming unusually quiet, complaining of stomach discomfort, or suddenly developing sensitivity to light or sound before the headache fully develops.
Many parents initially dismiss these early signs as typical childhood complaints or attempts to avoid schoolwork. However, recognizing these patterns as potential migraine warnings can prevent full-blown attacks and reduce their impact on a child's day. Teaching children to communicate these early sensations can be invaluable in managing their condition.
Understanding Physical Manifestations
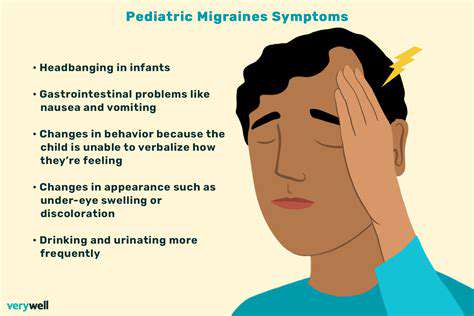
The physical symptoms of pediatric migraines extend beyond just head pain. Children might experience visual disturbances like seeing flashing lights or zigzag patterns before the headache starts—a phenomenon known as an aura. Other physical signs include pale skin, dark circles under the eyes, or sudden loss of appetite. Some children might even develop temporary speech difficulties or coordination problems during an attack.
These physical symptoms can be frightening for both children and parents, especially when they first appear. Documenting these occurrences helps healthcare providers understand the full picture of the child's condition and recommend appropriate treatments.
Assessing Emotional and Mental Changes
Migraines often bring noticeable changes in a child's mood and behavior. In the hours before an attack, some children become unusually irritable, anxious, or depressed. These emotional shifts, while sometimes mistaken for behavioral issues, can actually be important warning signs of an impending migraine. After the headache subsides, children might appear exhausted or emotionally drained.
Sleep disturbances are another common companion to pediatric migraines. Some children struggle to fall asleep before an attack, while others might sleep excessively afterward. Tracking these sleep pattern changes can provide valuable clues about migraine triggers and timing.
Monitoring Behavioral Patterns
Behavioral changes can serve as important indicators of migraine activity. Teachers might notice a typically attentive student suddenly struggling to concentrate or becoming unusually sensitive to classroom noise. Some children instinctively seek out dark, quiet spaces when they feel a migraine coming on—a behavior that should be recognized and accommodated.
Changes in academic performance or social interactions might also signal frequent migraine activity. Being alert to these behavioral shifts allows for timely intervention and necessary adjustments to the child's environment or schedule.
Seeking Professional Guidance
When migraine symptoms persist or significantly impact a child's life, professional medical advice becomes essential. Pediatric neurologists or headache specialists can offer specialized insights and treatment options. Delaying consultation can prolong a child's discomfort and potentially allow the condition to worsen. Modern diagnostic tools and treatment approaches have made managing pediatric migraines more effective than ever before.
Comprehensive evaluation might include keeping detailed headache diaries, blood tests to rule out other conditions, or in some cases, imaging studies. This thorough approach ensures accurate diagnosis and the most effective treatment plan.
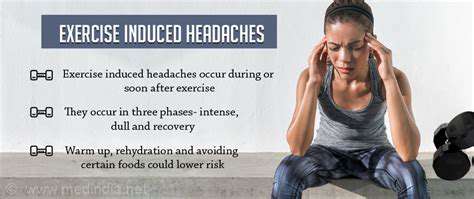
Lifestyle Factors and Prevention
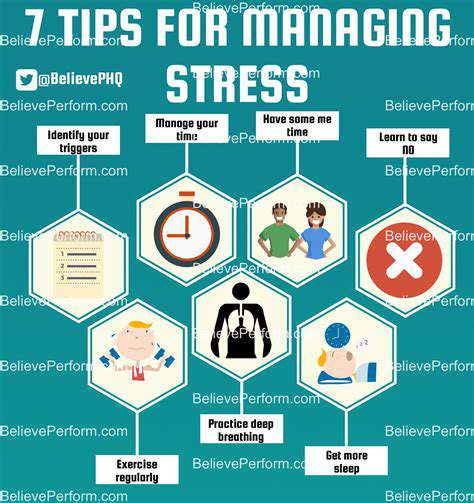
Preventive measures play a crucial role in managing pediatric migraines. Establishing consistent sleep routines, ensuring regular meals and hydration, and managing stress through age-appropriate techniques can all help reduce migraine frequency. Identifying and avoiding personal triggers—whether certain foods, environmental factors, or activities—can significantly decrease migraine occurrences.
Regular physical activity, within a child's tolerance level, can also be beneficial. Many children find that moderate exercise helps reduce stress and may decrease migraine frequency, though intense activity might trigger attacks in some cases. Finding the right balance is key.
Differentiating Pediatric Migraines from Other Headaches
Identifying the Signs and Symptoms
Distinguishing pediatric migraines from other childhood headaches requires understanding their unique characteristics. Unlike tension headaches that produce a dull, constant pressure, migraines typically cause pulsating pain that worsens with movement. The one-sided nature of the pain, combined with nausea and sensory sensitivities, helps differentiate migraines from other headache types. Children might describe the pain as pounding or like a heartbeat in my head.
Another distinguishing feature is the migraine's duration—typically lasting between 2 and 48 hours in children, compared to tension headaches which might come and go more quickly. The presence of associated symptoms like abdominal pain or visual disturbances further helps identify true migraines.
Understanding the Triggers
While many headaches share common triggers like stress or fatigue, migraine triggers tend to be more specific and consistent for each individual child. Food triggers like aged cheeses, processed meats, or foods containing MSG are more commonly associated with migraines than other headache types. Hormonal changes, particularly in adolescent girls, can also precipitate migraines more than other headaches.
Environmental factors like flickering lights, strong odors, or weather changes tend to affect migraine sufferers more significantly. Recognizing these personal triggers allows for better prevention and management compared to more generic headache types.
Differentiating from Other Pediatric Headaches
Cluster headaches, while less common in children, present with distinct symptoms—severe pain typically centered around one eye, often accompanied by tearing or nasal congestion on that side. Sinus headaches usually coincide with cold symptoms and produce pain concentrated in the sinus areas. Migraines, in contrast, typically don't show these localized symptoms and aren't necessarily tied to illness.
Another important distinction is how children respond during attacks. Migraine sufferers often want to lie still in a dark, quiet room, while children with tension headaches might continue activities despite discomfort. These behavioral differences can aid in accurate diagnosis.
The Role of Diagnostic Tools
While most pediatric migraines can be diagnosed through careful history-taking and examination, sometimes additional tests are needed to rule out other conditions. Neurological exams check for normal reflexes, coordination, and sensory responses. In cases with unusual features or concerning symptoms, imaging studies like MRI can help exclude rare but serious conditions that might mimic migraines.
Electroencephalograms (EEGs) might be considered if seizure activity is suspected, though they aren't routinely needed for typical migraine diagnosis. These tools help ensure accurate differentiation from other neurological conditions that might present similarly.
Management Strategies for Pediatric Migraines
Effective migraine management in children differs from approaches used for other headaches. While simple analgesics might suffice for tension headaches, migraines often require more specific treatments. Some children benefit from medications that target migraine-specific pathways, especially for frequent or severe attacks. Preventive medications might be considered when migraines significantly impact a child's life.
Non-pharmacological approaches like biofeedback, cognitive behavioral therapy, or relaxation techniques often prove particularly effective for pediatric migraines. Creating a personalized migraine toolkit with preferred comfort measures can empower children to manage their symptoms more effectively.
Pregnancy anxiety is a common experience for many expecting mothers. While unrelated to pediatric migraines, it shares the importance of early recognition and management. Understanding health conditions thoroughly leads to better outcomes whether dealing with migraines, anxiety, or other health concerns. Comprehensive approaches that address both physical symptoms and emotional well-being tend to be most successful.