Seasonal Allergies and Headaches: Is There a Link?
Inflammation: The Underlying Culprit
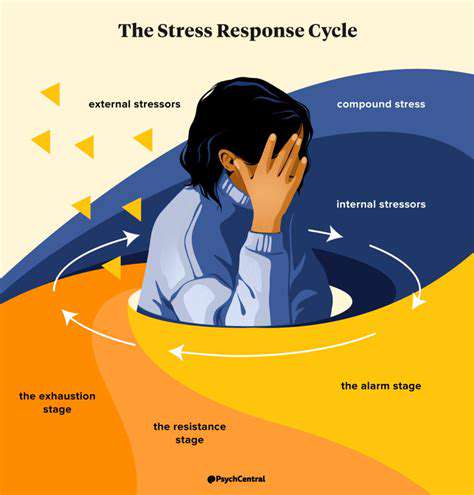
When our bodies face injury or infection, inflammation kicks in as a natural defense mechanism. This biological process mobilizes an army of cells and chemical messengers to neutralize threats and kickstart healing. But here's the catch - when inflammation overstays its welcome, it transforms from helpful defender to persistent troublemaker, often bringing along unwelcome guests like chronic pain.
Consider what happens during allergy season. The immune system sounds false alarms when harmless particles like pollen enter our system. This mistaken identity crisis triggers the release of inflammatory compounds including histamine and prostaglandins. While these chemicals aim to protect us, they're also responsible for those all-too-familiar allergy symptoms - from stuffy noses to relentless itching - and yes, they can even set the stage for headaches.
Allergens and the Immune System
Our immune systems sometimes behave like overzealous security guards, treating innocent pollen particles like dangerous intruders. This misidentification launches a full-scale defensive operation, complete with chemical weaponry that causes sneezing fits and watery eyes. What many don't realize is that this same biochemical warfare can directly contribute to headache development, creating an often-overlooked connection between seasonal sniffles and head pain.
The Role of Prostaglandins
Prostaglandins function like the body's chemical messengers with multiple responsibilities. During allergic reactions, certain prostaglandins get overproduced, acting like amplifiers for pain signals. These molecular troublemakers can target different pain receptors throughout our nervous system, explaining why allergy-related headaches can vary so much in their character and intensity.
The complex dance between allergens, immune responses, and prostaglandin production reveals why some people experience pounding headaches when pollen counts rise.
Neurological Pathways and Pain
Our nervous system acts like an intricate network of alarm wires. Inflammation can make these wires hypersensitive, causing them to fire pain signals at the slightest provocation. Allergic reactions can essentially short-circuit this system, potentially triggering headaches even without actual tissue damage. This neurological hypersensitivity helps explain why some individuals develop headaches during allergy season while others don't.
Headache Types and Allergic Triggers
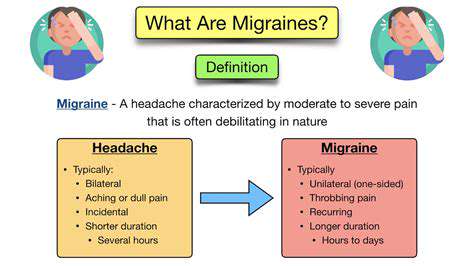
Allergy-related headaches come in various forms. Sinus headaches often accompany nasal congestion, creating pressure-like pain around the eyes and forehead. Some migraine sufferers report their attacks coincide with high pollen counts, suggesting allergies might lower their pain threshold. Recognizing these patterns can be crucial for effective treatment.
Inflammation's Impact on the Body
The ripple effects of allergic inflammation extend far beyond the nasal passages. This systemic response can create widespread discomfort that sometimes manifests as headaches. Understanding this whole-body perspective helps explain why managing allergies effectively might also reduce headache frequency for some individuals.
The Role of Histamine and Other Allergens
Histamine's Role in Allergic Reactions
Histamine acts as the body's chemical alarm system during allergic reactions. When mast cells detect allergens, they release histamine like tiny biological flares, triggering the classic allergy symptoms we all recognize. What's fascinating is how this same chemical can influence headache development through its effects on blood vessels and nerve endings.
The Allergen-Antibody Interaction
The allergy cascade begins when allergens encounter specialized IgE antibodies. This meeting triggers immune cells to release their chemical payloads, including histamine. It's this initial molecular handshake that sets the entire allergic reaction in motion, ultimately leading to symptoms that can include headaches.
Other Key Allergens in Seasonal Allergies
While pollen gets most of the attention, mold spores and dust mites can be equally troublesome. These microscopic triggers affect people differently - some react strongly to tree pollen but barely notice mold, while others have the opposite response. This variability makes allergy management highly personalized.
The Connection Between Allergens and Headaches
The headache-allergy link often goes unrecognized, yet for some individuals, managing their allergies effectively provides unexpected relief from chronic headaches. The inflammatory chemicals released during allergic reactions can affect blood vessels and nerves in ways that contribute to head pain.
Triggers Beyond Pollen: Mold and Dust Mites
While pollen dominates seasonal allergy discussions, mold spores thrive in damp environments year-round, and dust mites make themselves at home in our bedding and furniture. These persistent allergens can trigger symptoms similar to pollen allergies, including potential headache triggers.
The Inflammatory Cascade and Headache Development
The chemical storm unleashed during allergic reactions can directly impact headache development. Histamine and other mediators cause blood vessels to dilate, potentially creating pressure changes that register as pain. Simultaneously, these chemicals can sensitize nerve pathways, lowering pain thresholds.
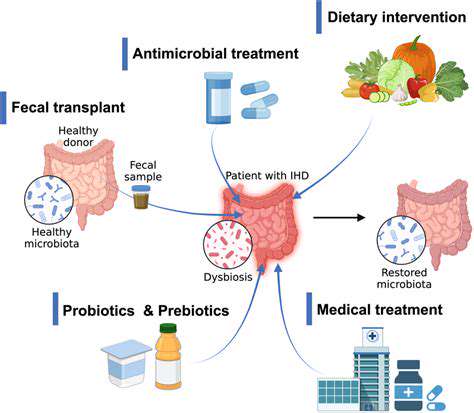
Management Strategies for Allergy-Related Headaches
Effective allergy control often brings headache relief. Beyond standard antihistamines, approaches like nasal irrigation, environmental controls, and immunotherapy can help break the allergy-headache cycle. For persistent cases, consulting an allergist can uncover specific triggers and tailor treatment accordingly.
Your posture significantly influences neck health. Proper ergonomic alignment can dramatically decrease neck strain and discomfort. Many office workers unknowingly adopt poor postural habits during long work hours. Simple adjustments like monitor positioning and regular movement breaks can make substantial differences in neck comfort over time.
Potential Symptoms and Types of Headaches
Potential Symptoms
Allergy-related headaches present with diverse symptoms that often overlap with other headache types. The telltale sign? Their timing coincides with allergy seasons or exposure to known triggers. The pain might feel like pressure building behind the eyes, a tight band around the forehead, or throbbing in the temples. Accompanying allergy symptoms - sneezing, itchy eyes, nasal congestion - often provide important diagnostic clues.
Different Types of Headaches Related to Allergies
Allergy sufferers might experience various headache forms. Tension-type headaches create steady, dull pressure, while migraines bring pulsating pain often accompanied by nausea and light sensitivity. Some report cluster headaches - severe, one-sided pain lasting weeks to months. Keeping detailed records of headache timing, characteristics, and associated allergy symptoms helps healthcare providers identify patterns and recommend appropriate treatments.