Sharp Neck Pain When Turning Head: Causes and Remedies
Understanding and Managing Neck Discomfort
Navigating Neck Health
Muscle overexertion frequently triggers acute neck discomfort
Disc displacement may lead to severe cervical distress
Body positioning habits significantly influence pain patterns
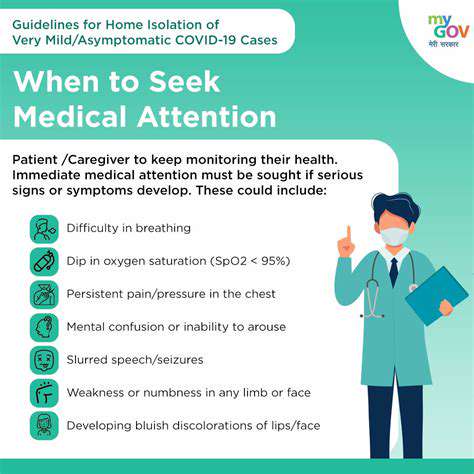
Medical consultation becomes crucial when sensory changes occur
Tracking symptom progression aids in timely intervention
Temperature-based therapies offer accessible relief options
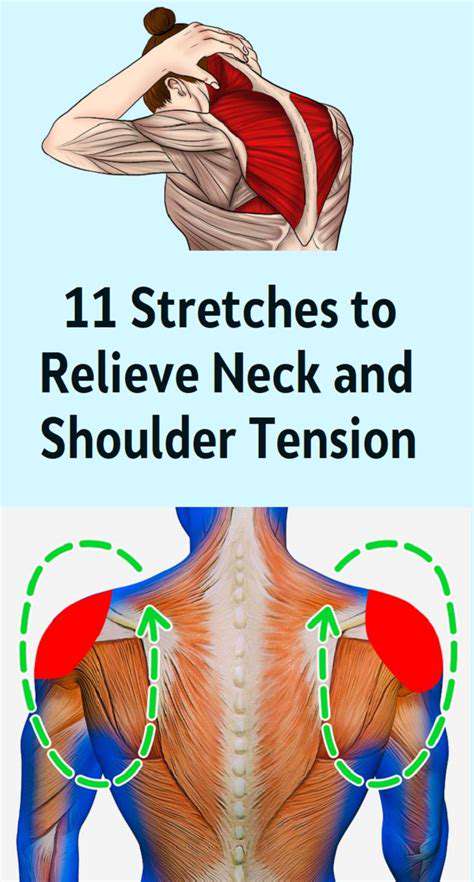
Mobility exercises enhance muscular elasticity
Workstation adjustments support spinal alignment
Sleep surface quality affects cervical recovery
Specialized care optimizes chronic condition management
Root Factors Behind Cervical Discomfort
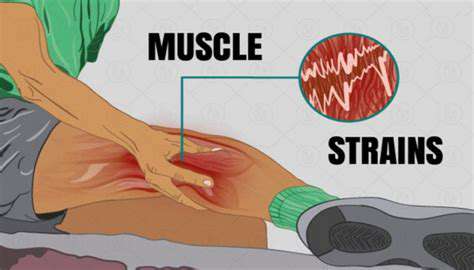
Muscular Overexertion and Fatigue
Neck muscles often bear the brunt of modern sedentary lifestyles. Prolonged screen use with improper head positioning creates cumulative stress on cervical structures. Office workers frequently develop tension patterns from maintaining static postures during extended computer sessions. The human head weighs approximately 10-12 pounds - when positioned forward just 15 degrees, the effective weight on neck muscles triples according to spine health research.
Unexpected movements during physical activities can create microtears in muscle fibers. Weekend athletes often report stiffness after unaccustomed exertion. Implementing dynamic warm-up routines before exercise sessions helps prepare tissues for activity demands. Listen to your body's warning signals - persistent discomfort during movement suggests the need for activity modification.
Disc-related Challenges and Neural Impingement
Cervical disc herniation affects approximately 2% of adults annually, with peak incidence between ages 40-50. This condition develops when intervertebral cushioning material protrudes beyond normal boundaries, potentially compressing adjacent nerve roots. Neural compression often manifests as electric-shock sensations radiating down the arms alongside localized neck stiffness.
Diagnostic imaging helps differentiate disc pathology from other conditions. Treatment protocols vary based on severity - from conservative approaches like traction therapy to surgical decompression in refractory cases. Recent studies highlight the effectiveness of combined physical therapy and anti-inflammatory regimens in managing 85% of disc-related cases without invasive procedures.
Articular Degeneration and Age-related Changes
Cervical osteoarthritis progression accelerates after age 50, affecting nearly 30% of the elderly population. Cartilage erosion in facet joints leads to bone-on-bone contact during movement, creating characteristic grinding sensations. Morning stiffness lasting over 30 minutes often signals degenerative joint changes requiring medical evaluation.
Management strategies focus on preserving mobility through low-impact exercises like swimming or tai chi. Synovial fluid production increases with regular movement, naturally lubricating affected joints. Some patients benefit from topical NSAID gels combined with manual therapy techniques to maintain functional range of motion.
Recognizing Critical Warning Signs
Red Flag Symptomatology
Neurological manifestations like limb numbness or loss of grip strength demand urgent assessment. These signs may indicate spinal cord compression or vascular compromise requiring immediate intervention. Track symptom patterns - pain intensifying at night or during rest periods often suggests non-mechanical origins needing specialized investigation.
Symptom Duration Considerations
Acute muscular strains typically resolve within 72 hours with proper care. Persistent discomfort beyond 96 hours warrants professional evaluation to rule out structural abnormalities. Chronic cases (lasting >12 weeks) often benefit from multidisciplinary pain management approaches combining physical rehabilitation with cognitive behavioral techniques.
Functional Impact Analysis
- Difficulty maintaining upright posture during routine activities
- Sleep pattern disruption due to positional discomfort
- Compromised work performance from concentration difficulties
Systemic Symptom Correlation
Concurrent manifestations like unexplained weight loss or night sweats may indicate neoplastic processes. Cervical lymphadenopathy with fever suggests infectious origins. Always disclose full medical history during consultations - previous trauma or inflammatory conditions significantly influence diagnostic pathways.
Practical Management Strategies
Immediate Relief Techniques
Contrast therapy (alternating heat/cold applications) effectively modulates acute inflammation. Begin with 15-minute ice pack applications to reduce swelling, followed by moist heat to improve tissue perfusion. Gentle isometric exercises maintain mobility without exacerbating inflammation - try pressing your palm against your forehead while gradually increasing resistance.
Ergonomic Optimization
Screen positioning should maintain the top third of monitors at eye level. Consider standing desk alternatives with anti-fatigue mats. Every 45 minutes of screen time should include 5 minutes of postural resetting exercises. Simple chin retractions (drawing the head backward without tilting) help counteract forward head posture.
Professional Interventions
Persistent cases may require targeted therapies like:
- Ultrasound-guided trigger point injections
- Graded motor imagery training for chronic pain
- Dry needling for myofascial release
Proactive Prevention Measures
Postural Reinforcement Techniques
Implement the wall test daily - stand with heels 6 inches from wall, ensuring shoulders and head touch the surface. Hold for 2 minutes while breathing deeply. This exercise reinforces proper spinal alignment and activates postural muscles.
Sleep Surface Optimization
Pillow height should maintain neutral cervical alignment - approximately 4-6 inches thickness depending on shoulder width. Side sleepers benefit from contoured memory foam pillows that fill the shoulder-neck gap. Mattress firmness should allow 2-3cm sinkage at hip/shoulder points while maintaining spinal neutrality.
Nutritional Support
Anti-inflammatory dietary patterns emphasizing omega-3 fatty acids (found in fatty fish) and turmeric supplementation may reduce musculoskeletal inflammation. Adequate magnesium intake (400mg daily) supports muscle relaxation - consider pumpkin seeds or dark leafy greens as natural sources.
Stress Management Integration
Chronic tension often manifests in cervical musculature. Diaphragmatic breathing exercises performed 3x daily significantly reduce muscular guarding behaviors. Progressive muscle relaxation techniques help break the pain-tension cycle common in chronic neck conditions.