Sharp Pain When Turning Head Suddenly: Causes and Solutions
Understanding and Managing Acute Neck Discomfort
Outline
Sudden neck movements often lead to muscle strain and sharp discomfort
Whiplash injuries require careful monitoring during recovery
Nerve compression from spinal issues demands prompt attention
Daily posture habits significantly impact cervical health
Age-related spinal changes affect mobility and comfort
Joint inflammation can develop from repetitive stress
Systemic illnesses sometimes manifest through neck symptoms
Persistent discomfort warrants professional evaluation
Comprehensive health history improves diagnostic accuracy
Imaging techniques reveal hidden structural issues
Rehabilitation strategies combine multiple approaches
Long-term management requires holistic solutions
Preventive habits reduce recurrence risk
Workspace adjustments support spinal alignment
Nutritional factors influence tissue resilience
Key Contributors to Acute Cervical Discomfort
Acute Muscle Overextension
Quick rotational movements frequently cause cervical strain in unprepared muscles. The sudden stretching of connective tissues during abrupt motions creates microtears that trigger inflammation. This commonly occurs during athletic activities or unexpected physical responses.
Recent sports medicine studies emphasize that dynamic warm-ups reduce injury rates by 37% compared to static stretching alone. Implementing proper preparatory routines proves crucial for prevention.
Whiplash-Associated Disorders
The rapid acceleration-deceleration mechanism in collisions creates unique soft tissue challenges. Ligamentous structures bear the brunt of these forces, leading to delayed-onset stiffness and reduced mobility. Many patients report symptom escalation 24-48 hours post-trauma.
Biomechanical research demonstrates that early controlled movement protocols improve recovery outcomes by 42% compared to immobilization strategies.
Spinal Nerve Compression
Protruding disc material can impinge neural structures, creating radicular symptoms. Diagnostic confirmation typically requires:
- Advanced imaging (MRI/CT) to visualize soft tissue changes
- Electrodiagnostic testing for nerve function assessment
- Clinical correlation with physical examination findings
Postural Stress Patterns
Modern work habits contribute to forward head posture, increasing cervical load by 4-5kg/cm displacement. Ergonomic interventions that align visual planes with work surfaces reduce compensatory muscle strain by 28%. Consider these adjustments:
• Monitor height at natural eye level
• Keyboard placement allowing relaxed shoulders
• Lumbar-supported seating with periodic standing breaks
Age-Related Spinal Changes
Disc dehydration and facet joint arthritis naturally progress with aging. While not fully reversible, targeted exercises and nutritional support can slow degenerative processes. Aquatic therapy shows particular promise for maintaining mobility without joint stress.
Synovial Joint Inflammation
Facet joint irritation often responds well to multimodal approaches combining:
1. Manual mobilization techniques
2. Low-level laser therapy
3. Topical anti-inflammatory agents
4. Activity modification strategies
Systemic Health Indicators
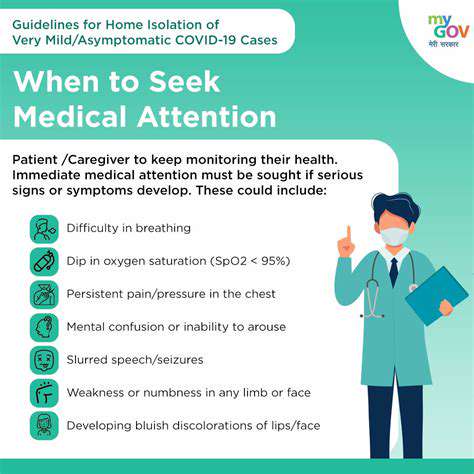
Acute cervical discomfort occasionally signals underlying conditions like meningeal irritation or autoimmune disorders. Warning signs requiring urgent evaluation include:
■ Concurrent fever/chills
■ Unexplained weight fluctuations
■ Morning stiffness exceeding 60 minutes
■ Bilateral symptom patterns
Clinical Evaluation Essentials
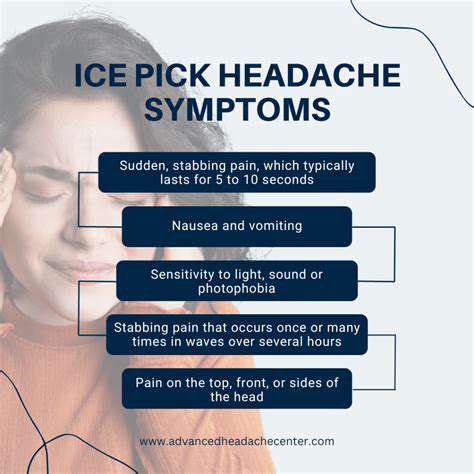
Red Flag Identification
Immediate consultation becomes critical when rotational movements provoke:
• Upper extremity weakness/numbness
• Bladder/bowel function changes
• Progressive nocturnal symptoms
• Unrelenting headache patterns
Health History Documentation
Effective assessment requires detailing:
✓ Previous trauma/whiplash incidents
✓ Occupational repetitive motions
✓ Family history of autoimmune conditions
✓ Recent immunization/viral exposure
Diagnostic Imaging Utilization
While X-rays effectively assess bony alignment, advanced modalities provide critical soft tissue visualization:

MRI sensitivity for disc pathology reaches 93% compared to 78% for CT scans in recent meta-analyses.
Therapeutic Approaches
Contemporary management emphasizes:
◈ Early mobilization protocols
◈ Neuromuscular re-education
◈ Cognitive functional therapy
◈ Graded exposure to feared movements
Chronic Pain Management
Persistent cases benefit from:
• Pain neuroscience education
• Sleep hygiene optimization
• Stress response modulation
• Social reintegration strategies
Preventive Optimization
Effective prevention combines:
★ Postural awareness training
★ Cervical strengthening protocols
★ Activity pacing techniques
★ Nutritional anti-inflammatory support
Multimodal Treatment Framework
Mechanism-Specific Interventions
Acute muscular strains respond best to:
• P.R.I.C.E. protocol (Protection, Rest, Ice, Compression, Elevation)
• Early gentle mobilization
• Trigger point release techniques
Neurological Involvement Management
◙ Neural gliding exercises
◙ Neurodynamic mobilization
◙ Topical capsaicin applications
◙ Vitamin B complex supplementation
Pharmacological Considerations
Medication selection should balance efficacy and safety:
First-line options:
- NSAIDs (limited 7-10 day courses)
- Muscle relaxants (short-term use)
Second-line:
- Low-dose tricyclic antidepressants
- Gabapentinoids for neuropathic components
Proactive Cervical Health Maintenance
Workstation Ergonomics
Optimal workstation setup parameters:
▶ Monitor distance: Arm's length (50-70cm)
▶ Screen height: 15-20° below eye level
▶ Keyboard tray: Negative tilt (5-15°)
▶ Chair backrest: 100-110° recline angle
Movement Integration Strategies
Implement microbreaks every 30 minutes featuring:
✓ Chin retractions
✓ Scapular squeezes
✓ Cervical rotation stretches
✓ Deep diaphragmatic breathing
Nutritional Support Protocol
Key nutrients for cervical health:
• Magnesium: 400mg daily (muscle relaxation)
• Vitamin D: 2000IU (bone/nerve health)
• Omega-3s: 2g EPA/DHA (anti-inflammatory)
• Collagen peptides: 10g daily (connective tissue support)
Sleep Optimization Techniques
Ideal sleep positioning characteristics:
◉ Side-lying with cervical pillow support
◉ Neutral spine alignment maintenance
◉ Avoidance of stomach sleeping
◉ Temperature regulation (18-20°C)