The Back of My Head Hurts: Understanding Causes and Relief
Common Causes of Pain at the Back of Your Head
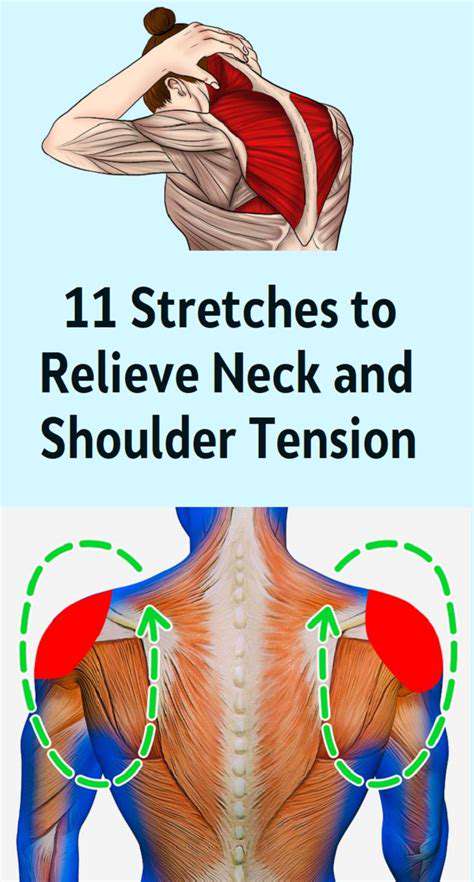
Muscle Strain and Tension
One of the most common causes of pain in the back of your head is Muscle Strain. This can occur due to poor posture or extended hours spent in front of a computer or phone. Poor ergonomic setups promote tension in the neck and shoulder muscles, leading to discomfort. Furthermore, stress and anxiety can exacerbate muscle tension, contributing to persistent pain.
Engaging in activities that strain the upper body, such as heavy lifting or intense workouts, can also lead to soreness in this area. It’s essential to take breaks and stretch regularly to alleviate this tension.
Recognizing the signs of muscle strain is crucial for timely intervention. Symptoms may include localized pain, stiffness, and sensitivity in the neck and shoulder region. If left unaddressed, muscle strain can escalate into more severe headaches and discomfort.
Consulting a healthcare professional can provide insights into personalized stretch routines. In many cases, physical therapy may offer relief and improve overall posture.
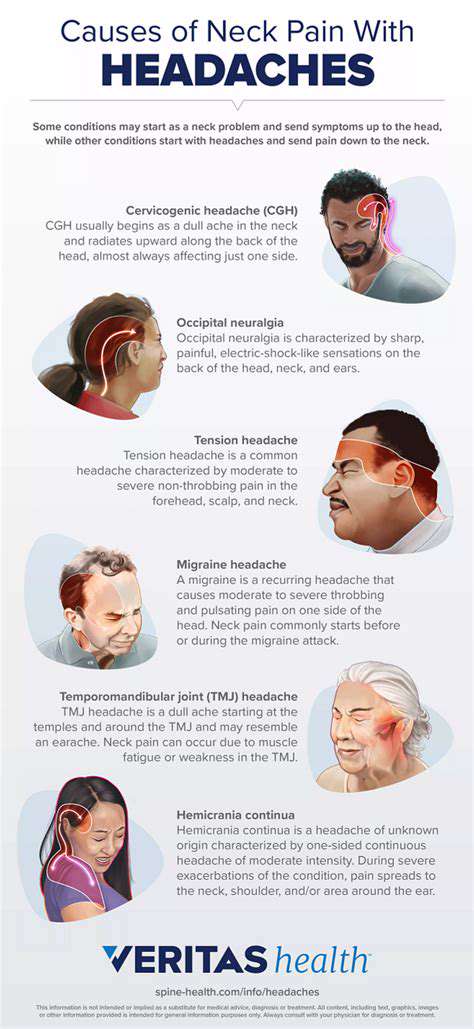
Migraine and Tension Headaches
Migraines are a type of headache that can cause extreme pain, often located at the back of the head. These headaches are often accompanied by nausea, light sensitivity, and aura symptoms. Understanding individual triggers is vital for managing migraines effectively. Common triggers may include certain foods, hormonal changes, and environmental factors.
Tension headaches, on the other hand, may present more subtly, often causing dull, aching pain. They can be a result of stress, lack of sleep, or prolonged screens. While migraines are generally more severe and may require medication, tension headaches can usually be managed with lifestyle changes.
Identifying the type of headache you experience is critical for targeted treatment. Keeping a headache diary can aid in determining patterns and triggers. If headaches persist, consultation with a healthcare provider is recommended for further evaluation.
Moreover, both types of headaches can sometimes coexist, leading to compounded discomfort. Therefore, a comprehensive treatment strategy is often required for relief from both conditions.
Cervical Spine Issues
Problems related to the cervical spine, including herniated discs or arthritis, can lead to pain radiating to the back of the head. These conditions can compress nerves, causing discomfort that may mimic headaches. Early diagnosis is key in addressing spinal issues effectively. Regular check-ups can help detect any underlying conditions before they worsen.
Injuries from accidents or falls can also contribute significantly to neck pain and headaches. Treatment options may include physical therapy, chiropractic care, or medication to manage inflammation. Staying active and maintaining a healthy lifestyle can support spinal health.
Additionally, it's essential to practice good posture, especially while sitting for long periods. Ergonomic chairs and desks can significantly minimize strain on the cervical spine. If you begin to experience chronic pain, an evaluation by a specialist can provide insight.
Taking preventive measures can avoid many spine-related issues. Regular exercise, proper sleep positions, and mindful ergonomics can create a healthier foundation for your spine.
Sinus Issues and Infections
Sinus infections can cause significant pressure and pain in the back of the head. When sinuses swell due to infection or allergies, pain can radiate from the sinuses to the surrounding areas, including the neck. Being aware of sinus symptoms is crucial for seeking timely treatment. Symptoms may include nasal congestion, fever, and facial pain along with headaches.
Preventative measures include managing allergens and maintaining good nasal hygiene. Neti pots or saline sprays can help keep sinuses clear. If allergies play a role, antihistamines might provide relief from headaches.
Consulting with a healthcare provider for recurrent sinusitis can lead to tailored interventions. In some cases, chronic sinusitis may require surgical solutions for long-term relief. Staying hydrated and practicing steam inhalation can provide immediate comfort during sinus infections.
Timely treatment of sinus issues can prevent complications that may exacerbate headaches and discomfort. Therefore, taking sinus health seriously is essential for overall well-being.
Other Potential Factors
Other factors contributing to pain at the back of the head can include environmental ones, such as loud noises or bright lights. For some individuals, changes in the weather can trigger discomfort as well. It’s essential to recognize external stimuli that affect head pain. Avoiding known triggers can help manage and reduce headache occurrences.
Additionally, dehydration is often an overlooked cause. Failure to drink enough water throughout the day can lead to headaches and general fatigue. It’s vital to prioritize hydration, particularly during hot days or when engaging in physical activity.
Sleep quality can also significantly influence headache frequency and severity. Poor sleep patterns contribute to overall body tension, which can lead to pain. Incorporating good sleep hygiene practices can foster better rest and lower headache incidents.
Lastly, hormonal changes can impact headache patterns, especially in women. Tracking cycles and symptoms can help identify hormonal triggers, providing opportunities for proactive responses. Understanding these various factors can facilitate a comprehensive approach to managing pain at the back of the head.
Tension Headaches
What are Tension Headaches?
Tension headaches are the most common type of headache, often described as a feeling of pressure or tightness around the forehead or back of the head. These headaches can vary in intensity but typically range from mild to moderate. Unlike migraines, which can be debilitating, tension headaches tend to be less severe and are often more manageable.
The key symptom of a tension headache is a persistent dull ache that can affect both sides of the head. Sufferers might also experience tenderness in the scalp, neck, and shoulder muscles. While the exact cause remains unclear, they are often triggered by stress, poor posture, or muscle strain.
Common Triggers of Tension Headaches
Various factors can precipitate a tension headache, with stress being one of the leading causes. Emotional stress from work, relationships, or personal issues can lead to muscle tension in the head, neck, and shoulders. Additionally, physical strain such as improper posture while working or sitting for extended periods can contribute significantly.
Other triggers include inadequate hydration, fatigue, and skipping meals. Environmental factors like bright lights or noise can aggravate the condition as well. Recognizing these triggers can help individuals take proactive measures to prevent headaches from occurring.
Management and Relief Techniques
Managing tension headaches often involves addressing the root causes. Techniques such as stress management, regular exercise, and maintaining a consistent sleep schedule can be beneficial. Practicing relaxation techniques such as deep breathing, meditation, or yoga can also help relieve built-up stress and tension.
Over-the-counter pain relief medicines, such as ibuprofen or acetaminophen, can effectively alleviate symptoms for many people. However, individuals who suffer from chronic tension headaches should consult a healthcare professional for a tailored treatment plan that may include physical therapy or other therapeutic options.
When to Seek Medical Attention
While tension headaches are generally not a cause for serious concern, it’s crucial to pay attention to their frequency and intensity. If headaches become chronic, interfere with daily activities, or are accompanied by additional symptoms such as visual disturbances, nausea, or significant changes in character, it is advisable to seek medical evaluation.
Healthcare professionals can help differentiate between tension headaches and other headache types that may require different treatments, such as migraines or cluster headaches. Early intervention can lead to more effective management strategies and improved quality of life.
Chronic Neck Pain

Understanding Chronic Neck Pain
Chronic Neck Pain is a common issue that affects many individuals, and it can significantly impact daily life. The causes of chronic neck pain often include poor posture, repetitive strain, and injuries. It is crucial to identify the underlying factors contributing to neck pain to effectively manage it. Some medical conditions, such as herniated discs and arthritis, can also lead to persistent discomfort. Knowing the symptoms associated with chronic neck pain is the first step toward seeking appropriate treatment.
Patients experiencing chronic neck pain may also suffer from accompanying symptoms like headaches and shoulder discomfort. Such pain can often be exacerbated by stress, leading to muscle tension in the neck area. Understanding the interconnection between these symptoms is vital for comprehensive treatment. Physical therapy and corrective exercises can be beneficial in alleviating these symptoms and improving overall neck function. Seeking professional guidance will help patients develop personalized treatment plans.
Additionally, lifestyle choices play a significant role in neck health. Lack of physical activity, poor ergonomics while working, and inadequate sleep can contribute to chronic neck pain. Regular stretching and strengthening exercises can help maintain a healthy neck and prevent further issues. Staying aware of body mechanics, especially during repetitive tasks, can reduce the likelihood of developing chronic pain.
In summary, chronic neck pain is a multifaceted issue that requires a thorough understanding of its causes and effects. By addressing lifestyle factors and seeking medical intervention when necessary, individuals can find relief from their pain and improve their quality of life. Ongoing education about proper body mechanics and self-care techniques is essential for preventing the recurrence of neck issues.
Treatment Options for Chronic Neck Pain
There are various treatment options available for managing chronic neck pain, each tailored to individual needs. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can provide temporary relief from discomfort. For more severe pain, physicians may prescribe stronger medications, including muscle relaxants. It is essential to consult with a healthcare provider to determine the most appropriate pain management strategy.
Physical therapy is another widely used approach for treating chronic neck pain. A trained therapist can teach patients exercises designed to strengthen neck muscles and improve flexibility. Techniques such as heat therapy, ultrasound, and electrical stimulation may also be utilized to reduce pain and promote healing. Maintaining consistency in therapy is crucial to maximize its benefits.
In some cases, alternative therapies like chiropractic adjustments and acupuncture can offer relief. These treatments aim to address spinal alignment and restore balance to the body. While some individuals may find these methods effective, it is essential to approach alternative therapies with caution and seek qualified practitioners. Ensuring that any treatment is safe and suitable for one's specific condition is vital.
Surgery may be considered a last resort for patients who do not find relief through conservative treatments. Procedures such as spinal fusion or discectomy can provide long-term solutions for chronic neck pain resulting from structural issues. Patients should thoroughly discuss the potential risks and benefits of surgery with their healthcare team. In many cases, a combination of treatments can provide the best outcomes.
Self-Care Techniques for Neck Pain Management
Self-care techniques can play a significant role in managing chronic neck pain. Regularly practicing good posture while sitting, standing, and sleeping can alleviate strain on the neck. Utilizing ergonomic furniture, such as chairs and desks that promote proper alignment, is also recommended. Incorporating breaks throughout the day to stretch and move can help reduce tension.
Heat and cold therapy are effective methods for self-management of neck pain. Applying heat increases blood flow and relaxes stiff muscles, while cold therapy numbs the area and reduces inflammation. Alternating between these therapies can provide comprehensive relief and aid in recovery. Individuals should pay attention to their bodies and modify self-care routines as needed.
Stress management techniques, including mindfulness meditation and deep breathing exercises, can help alleviate neck pain associated with tension. Incorporating relaxation practices into daily routines can contribute to overall well-being. Maintaining a balanced diet and staying hydrated supports muscle function and helps prevent stiffness and discomfort.
Finally, keeping a pain diary to track pain levels and triggers can assist patients in identifying patterns and managing their condition effectively. This record can be shared with healthcare providers to tailor treatment approaches. By taking an active role in self-care, patients can empower themselves to manage chronic neck pain more effectively.
When to Seek Professional Help
Knowing when to seek professional help for chronic neck pain is vital for effective treatment. If pain persists for more than a few weeks, it may be a sign of a more serious condition that requires medical evaluation. Other red flags include numbness, tingling, or weakness in the arms or hands, which could indicate nerve involvement. Prompt medical attention can prevent further complications and facilitate quicker recovery.
Additionally, if neck pain develops after a traumatic injury, such as a fall or car accident, it is crucial to seek medical care immediately. Imaging studies, such as X-rays or MRIs, may be necessary to assess the extent of potential injuries. Healthcare providers can offer personalized treatment options based on the specific diagnosis and identified issues.
Patients should also consult a doctor if neck pain is accompanied by fever, unexplained weight loss, or severe headaches. These symptoms may signal underlying health concerns that require prompt intervention. Regular check-ins with healthcare providers can help monitor progress and adjust treatment plans accordingly.
In conclusion, understanding the intricacies of chronic neck pain, recognizing when to seek help, and employing self-care techniques can significantly impact an individual's quality of life. Patients should remain proactive in managing their condition and maintain open communication with their healthcare teams. Collaboration in the treatment process is essential for achieving lasting relief and improved well-being.
Occipital Neuralgia
What is Occipital Neuralgia?
Occipital neuralgia is a condition characterized by sharp, jabbing pain that often originates from the back of the head and can radiate towards the front or down the neck. This type of pain is typically linked to irritation or injury of the occipital nerves, which run from the top of the spinal cord up through the scalp.
People suffering from occipital neuralgia often describe the pain as similar to sudden electric shocks, making it difficult to focus or perform daily tasks. The intensity and frequency of these episodes can vary from person to person.
Identifying occipital neuralgia can be challenging, as its symptoms can mimic those of other headache disorders, such as migraines or tension headaches. Proper diagnosis is crucial for effective treatment and pain management.
Causes of Occipital Neuralgia
Many factors can contribute to the development of occipital neuralgia. One common cause is muscle tension or spasms in the neck, which can irritate the occipital nerves. This tension can arise from poor posture, stress, or repetitive strain injuries.
Injuries to the neck, including whiplash or trauma from accidents, may also trigger this condition. Such injuries can cause inflammation or nerve compression, leading to the characteristic pain associated with occipital neuralgia.
Underlying medical conditions, such as diabetes or gout, can predispose individuals to nerve damage and increase the risk of occipital neuralgia. In some cases, an infection or structural issues in the spine may also play a role in developing the condition.
Symptoms and Diagnosis
The primary symptom of occipital neuralgia is a shooting or stabbing pain at the back of the head, which may be on one side or both sides. This pain can be accompanied by tenderness in the scalp and may worsen with neck movement or pressure.
In addition to pain, individuals with occipital neuralgia may experience other sensations, such as throbbing headaches or sensitivity to light. Migraine-like symptoms, including nausea and visual disturbances, can also occur in some cases.
To diagnose occipital neuralgia, healthcare providers will often conduct a thorough physical examination and review the patient’s medical history. Imaging tests, such as MRI or CT scans, may be ordered to rule out other conditions and confirm the diagnosis.
Treatment Options
Treatment for occipital neuralgia can vary based on the severity and underlying causes of the condition. Initial approaches often include conservative methods, such as physical therapy, heat or cold therapy, and gentle stretching exercises to relieve muscle tension.
Medications, including anti-inflammatory drugs, muscle relaxants, and nerve blocks, may be prescribed to manage pain effectively. In more severe cases, stronger pain medications or antidepressants that help alleviate nerve pain may be considered.
For individuals who do not respond to conservative treatments, procedures like occipital nerve stimulation or Botox injections may offer relief. Surgical options are generally seen as a last resort for chronic sufferers who do not find relief from other methods.
Managing Occipital Neuralgia
Living with occipital neuralgia can be challenging, but several strategies can help manage symptoms and improve quality of life. Maintaining a proper posture while working or engaging in everyday activities is essential to minimize neck strain.
Incorporating regular physical exercises, such as yoga or stretching, can help relieve muscle tension in the neck and shoulders. Mindfulness practices, such as meditation or deep-breathing exercises, may also reduce stress and contribute to overall well-being.
Keeping a pain diary can assist individuals in identifying triggers and patterns related to their occipital neuralgia, allowing for better management strategies. Sharing this information with healthcare providers can lead to more personalized treatment plans and improved outcomes.
Increased Stress and Anxiety
Physical Symptoms of Stress
Increased stress levels can lead to a variety of physical symptoms, one of which is pain or discomfort in the back of the head. This can manifest as tension headaches, which are caused by the contraction of muscles in the neck and scalp. The pain may feel like a tight band around the head, and it can vary in intensity.
Additionally, stress may contribute to bruxism, a condition where individuals grind or clench their teeth, often subconsciously, particularly during sleep. This action can lead to significant discomfort in the jaw and neck muscles, indirectly causing pain at the back of the head.
Chronic stress can also exacerbate existing medical conditions such as migraines, which can present as severe throbbing pain, often focused on one side of the head but potentially radiating to the back. Understanding the interplay between stress and these conditions is vital for effective pain management.
Posture is another aspect affected by stress. When we are anxious or under pressure, we may unconsciously tense our shoulders and neck, leading to muscle fatigue and pain, including discomfort at the back of the head. Proper ergonomic practices are essential in mitigating these effects.
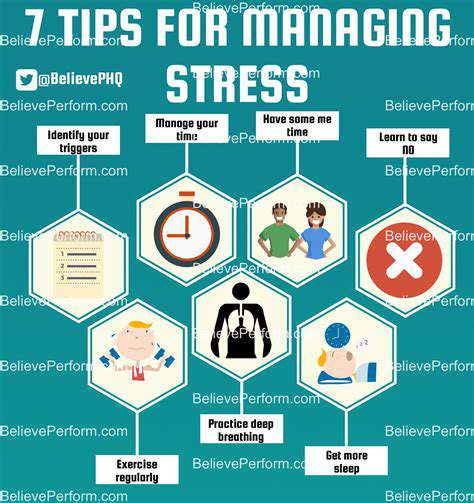
It's important for individuals experiencing back-of-head pain related to stress to recognize the signs and explore relaxation techniques. Practices such as deep breathing, yoga, and meditation can significantly help in alleviating stress-related symptoms.
Identifying Stress Triggers
To effectively manage Stress-related Pain, it is crucial to identify personal stress triggers. These can range from workplace pressures, academic responsibilities, or personal relationships to significant life changes like moving or job transitions. Understanding these factors can empower individuals to address their sources of stress proactively.
Journaling is a helpful exercise in pinpointing triggers. By documenting daily events alongside pain levels and emotions, individuals can identify patterns that correlate with increased stress and discomfort. This awareness allows for targeted strategies to address those triggers.
In addition to journaling, mindfulness practices can aid in recognizing physical and emotional stress responses. Mindfulness encourages present-moment awareness, making it easier to identify when stress levels are rising and to implement coping mechanisms immediately.
Building a support network is also an effective way to manage triggers. Sharing experiences with friends, family, or professionals can provide perspective and validation, which may lessen the psychological burden and alleviate physical symptoms over time.
It's essential to approach stress management holistically. Regular physical activity, adequate sleep, and a balanced diet play significant roles in moderating stress responses and preventing physical symptoms, including pain in the back of the head.
Strategies for Relief
Relieving stress-related pain often requires a multi-faceted approach. One effective strategy is incorporating relaxation techniques into daily routines. Practices such as deep breathing exercises, progressive muscle relaxation, or guided imagery can help regulate the body's stress response and decrease tension in the muscles.
Regular physical exercise is another powerful tool for managing stress. Activities such as jogging, yoga, or swimming not only improve physical health but also release endorphins, which act as natural painkillers and mood elevators. Aim for at least 30 minutes of moderate exercise most days of the week.
In addition to physical activity, ensuring proper hydration and nutrition can contribute to overall well-being. Dehydration can lead to headaches and increased pain perception, while a balanced diet rich in omega-3 fatty acids, vitamins B and C, and antioxidants can support brain health and stress management.
Seeking professional help, including therapy or counseling, can provide additional support for individuals struggling with stress. Cognitive-behavioral therapy (CBT) has proven effective in addressing anxiety and stress, helping individuals develop coping strategies tailored to their specific needs.
Using complementary techniques such as acupuncture or massage therapy can also be highly beneficial. These methods can relieve tension in the muscles, improve blood flow, and promote relaxation, all of which contribute to decreasing discomfort at the back of the head.
The Importance of Self-Care
Practicing self-care is essential for maintaining mental and physical health, especially in the context of increased stress and anxiety. Setting aside dedicated time for self-care activities such as reading, taking a warm bath, or pursuing hobbies can provide the necessary respite to recharge emotionally and physically.
Cultivating a balanced lifestyle that includes quality sleep, nutritious meals, and leisure activities is vital in managing stress levels. Establishing a consistent sleep schedule can significantly impact stress reduction and overall well-being, while adequate nutrition sustains energy and mood balance.
Mindfulness and meditation offer powerful self-care options that promote relaxation and emotional resilience. Even a few minutes of mindfulness practice each day can help reduce symptoms of anxiety and provide clarity when facing stressors.
Being mindful of the media consumed can also aid in stress management. Limiting exposure to negative news cycles and seeking out positive content, such as uplifting podcasts or inspirational books, can influence mental health positively.
Ultimately, prioritizing self-care fosters resilience against stress-related pain. By consciously integrating self-care practices into daily life, individuals can experience profound improvements in their stress levels and overall health, which will alleviate symptoms, including discomfort at the back of the head.
Possible Allergies or Sinusitis

Identifying Symptoms of Allergies and Sinusitis
Allergies often present themselves through various symptoms, including sneezing, runny nose, and itchy eyes. Understanding the full spectrum of symptoms can help you determine if allergies are the underlying cause of your discomfort. In contrast, sinusitis typically involves nasal congestion, facial pain, and headaches.
While allergies may trigger a quick response, sinusitis can develop over time, making it crucial to recognize its chronic form. Long-term exposure to allergens can lead to persistent sinus issues, worsening your overall health. Observing these symptoms over time can guide you towards proper treatment.
It is beneficial to maintain a symptom diary, noting occurrences and potential triggers, to aid in identifying whether allergies or sinusitis are at play. Consult a healthcare professional if symptoms intensify or persist, as they can provide tailored advice for your situation.
Finding Relief Through Treatment Options
Managing allergies and sinusitis often requires a multifaceted approach. Over-the-counter medications such as antihistamines may offer immediate relief for allergic reactions. Additionally, decongestants can alleviate sinus pressure and improve breathing.
In some cases, home remedies like nasal irrigation or steam inhalation can also be helpful. Staying hydrated and using a humidifier are simple ways to soothe irritated nasal passages. These methods work together to clear congestion and provide comfort.
Consulting a healthcare provider for more severe cases can lead to prescription medications or allergy testing. Understanding your specific condition allows for more effective treatment strategies. Your doctor may recommend immunotherapy or more advanced procedures if allergies or sinusitis become chronic.
Preventive Measures to Minimize Discomfort
Preventing allergies and sinusitis starts with awareness of environmental triggers. Regular cleaning can help reduce dust and mold levels in your home, while using air purifiers can improve overall air quality. Taking steps to minimize allergens can significantly reduce the chance of flare-ups.
Avoidance strategies also play a crucial role. Staying indoors during high pollen counts or wearing masks in polluted environments can help shield your respiratory system. Keeping windows shut and using air conditioning can further protect against outdoor allergens.
Lastly, maintaining a healthy lifestyle—rich in vitamins, minerals, and hydration—can strengthen your immune system, making it more resilient against allergens and infections. Regular check-ups with your healthcare provider can also ensure that your preventive measures are effective.
When to Seek Medical Attention
Recognizing Severe Symptoms
When experiencing pain at the back of the head, it is crucial to differentiate between mild discomfort and more Severe Symptoms. Severe symptoms can include intense, persistent pain that does not respond to over-the-counter medications.
Other alarming signs may include sudden vision changes, loss of balance, or confusion. If these symptoms arise, it is essential to seek immediate medical attention, as they could indicate a serious underlying condition.
A high fever accompanied by neck stiffness may also signal the presence of meningitis, which is a medical emergency. Don't hesitate to reach out to a healthcare provider if you experience this combination of symptoms.
Always trust your instincts; if something feels off, it is better to err on the side of caution and consult with a medical professional.
When Pain Persists
If the pain at the back of your head persists for more than a few days, seeking medical advice becomes necessary. Chronic headaches or migraines may require specialized treatment plans to manage effectively.
It is also important to note if the pain worsens with certain movements or positions, as this could indicate a specific issue that needs addressing. A doctor may recommend imaging studies, such as an MRI or CT scan, to understand the root cause better.
In chronic cases, a neurologist might be involved in your care. They can provide insights into potential triggers and suggest various treatment options including lifestyle changes, medications, or alternative therapies.
Documenting your symptoms and their severity can provide valuable information during your medical consultation, aiding in timely and accurate diagnosis.
Understanding Risk Factors
Certain risk factors can increase the likelihood of experiencing pain at the back of your head. These factors include high-stress levels, poor posture, and sedentary lifestyles, which can contribute to tension headaches.
Additionally, individuals with a history of migraines or tension-type headaches may find that these conditions flare up more frequently. Lifestyle choices, such as inadequate hydration or poor sleep quality, can also exacerbate existing pain issues.
For some, underlying health conditions like hypertension or cervical spine disorders may significantly contribute to headache pain. Regular check-ups and screenings can help identify these risk factors early on.
Understanding your personal risk factors is vital not just for treatment but for prevention. Engaging in healthy lifestyle practices such as regular exercise, a balanced diet, and effective stress management techniques can reduce the frequency and severity of headaches.