The Role of Hormonal Fluctuations as Migraine Triggers
- Estrogen's effect on serotonin levels
- Progesterone's influence on blood vessel dilation
- Cortisol's impact on pain thresholds
The Societal Impact
Hormonal headaches disproportionately affect women, with significant workplace and economic consequences. Studies estimate that menstrual-related migraines alone cost billions annually in lost productivity. Yet this health issue often remains under-recognized in workplace policies and medical research funding.
The stigma surrounding women's health issues has historically limited research into these conditions. Only recently have large-scale studies begun properly investigating hormonal headache mechanisms and treatments.
The Personal Experience
For individuals experiencing hormonal headaches, the condition often follows predictable monthly patterns. Many report:
- Increased sensitivity to light and sound
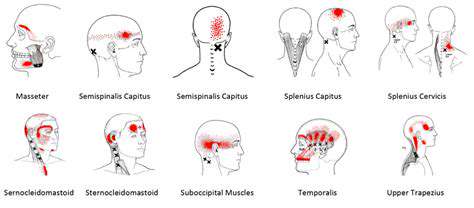
- Distinct pain locations (often unilateral)
- Associated nausea and fatigue
The Future Implications
Emerging technologies offer hope for better management:
- Wearable hormone monitors
- Personalized medication regimens
- Advanced neuroimaging techniques
Progesterone's Influence on Migraine Attacks
Progesterone and the Menstrual Cycle
Progesterone levels follow a predictable pattern during the menstrual cycle, peaking in the luteal phase before declining sharply if pregnancy doesn't occur. This decline appears particularly significant for migraine sufferers, with many women reporting headaches in the days leading up to menstruation.
Interestingly, some women find their migraines improve during pregnancy when progesterone levels remain consistently high. This observation has led researchers to investigate whether stable progesterone levels might be protective against migraines.
Migraine Triggers and Hormonal Shifts
The relationship between progesterone and migraines isn't straightforward. While some women experience migraines when progesterone drops, others are more sensitive to estrogen fluctuations. Key factors include:
- Rate of hormone level change
- Absolute hormone levels
- Individual sensitivity thresholds
Progesterone's Role in the Brain
Progesterone metabolites interact with GABA receptors, potentially explaining some of its neurological effects. The hormone also influences:
- Neurotransmitter balance
- Cerebral blood flow
- Inflammatory responses
The Influence of Estrogen and Progesterone Interactions
The estrogen-progesterone ratio appears more important than absolute levels for many women. Some key observations:
- High estrogen with low progesterone often triggers migraines
- Balanced ratios tend to be protective
- Individual optimal ratios vary significantly
Potential Mechanisms of Action
Current research focuses on several pathways:
- Blood vessel modulation in meninges
- Trigeminal nerve sensitization
- Inflammatory mediator release
- Central pain processing changes
Clinical Implications and Future Research
Practical applications of this research include:
- Timed hormone supplementation
- Cycle-based preventive medications
- Personalized contraceptive choices
Other Hormonal Factors and Migraine Triggers
Progesterone Fluctuations
The luteal phase progesterone drop isn't the only significant fluctuation. Other important periods include:
- Post-ovulation rise
- Early pregnancy increases
- Perimenopausal variations
Estrogen and Migraine
Estrogen's effects are similarly complex:
- Helps regulate pain pathways
- Affects serotonin availability
- Modulates blood vessel tone
- During menstruation
- With placebo pills in birth control packs
- In the postpartum period
Thyroid Hormones
Thyroid disorders can mimic or exacerbate migraines through:
- Altered metabolic rates
- Changed blood flow patterns
- Modified pain perception
Stress Hormones and Migraine
The stress-migraine connection involves multiple pathways:
- Cortisol's anti-inflammatory effects
- Adrenaline's vascular impacts
- HPA axis dysregulation